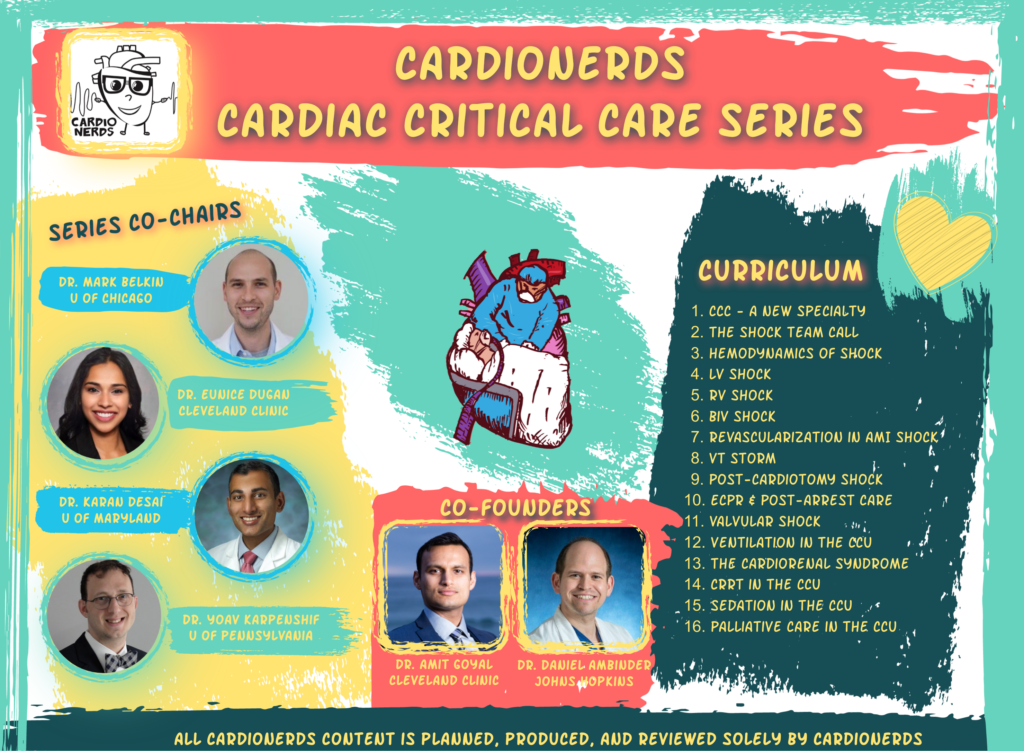
Cardionerds: A Cardiology Podcast
Cardionerds: A Cardiology Podcast 168. CCC: Cardiogenic Shock – Initial Assessment and The Shock Team Call with Dr. Anu Lala
Clinical Definition And Hemodynamic Criteria
- Cardiogenic shock is defined by hypotension, end-organ hypoperfusion, and specific hemodynamics.
- Classic hemodynamic cutoffs include CI ≤2.2 L/min/m2 and PCWP ≥15 mmHg alongside clinical hypoperfusion.
Start With A Focused Bedside Exam
- Do a focused bedside exam and build a human connection while assessing the patient.
- Use pulses, temperature, JVP, PMI, heart sounds, and hourly urine output to evaluate perfusion and congestion.
Prioritize Trends Over Single Measurements
- Track trends in urine output, lactate, and blood pressure rather than relying on single values.
- Trends better reflect response to therapy and the patient's true trajectory in shock.
Cardiogenic shock is a state of cardiac dysfunction leading to hemodynamic instability and end-organ hypoperfusion. At the bedside, clinicians take various data points – from history to physical exam to labs/imaging and invasive hemodynamics – to make an assessment of the etiology, severity and management of cardiogenic shock. Health systems have developed “Shock Teams” to collectively interpret this data to deliver the optimal care for each patient. In this episode, Dr. Mark Dela Cruz (Advanced Heart Failure and Transplant Fellow at University of Chicago), CardioNerds Critical Care Series Co-Chairs Dr. Mark Belkin (Advanced Heart Failure and Transplant Fellow at University of Chicago) and Dr. Karan Desai (General Cardiology Fellow at University of Maryland), and CardioNerds Co-Founder Dr. Daniel Ambinder (Structural Fellow at Johns Hopkins Hospital) join Dr. Anu Lala (Director of the AHFT Fellowship, Associate Professor of Medicine and Cardiology at Mount Sinai Hospital and Deputy Editor of the Journal of Cardiac Failure) on a Shock Team Call! Dr. Lala leads us in a discussion of the systematic bedside evaluation of cardiogenic shock, from understanding a patient’s physiology and their humanity, to manage their illness and make a rapid but thorough evaluation when on the Shock Call. Audio editing and episode introduction by CardioNerds Academy Intern, Hirsh Elhence.
Claim free CME for enjoying this episode! Disclosures: None
Pearls • Notes • References • Guest Profiles • Production Team
Pearls and Quotes – Shock Team Call
- The classic definition of cardiogenic shock was derived from studies of left ventricular dysfunction in the setting of acute myocardial infarction. With the advent of early primary percutaneous coronary intervention (PCI) and trends in cardiovascular disease risk factors, the prevalence of non-ischemic etiologies of cardiogenic shock (e.g., progression/exacerbation of chronic heart failure) has increased significantly.
- The diagnosis of cardiogenic shock should be made by integrating key clinical features such as physical exam findings and objective laboratory and imaging data in an iterative fashion. Focused transthoracic echocardiography and invasive hemodynamics are helpful in further characterizing the type of shock and the etiology of cardiogenic shock.
- Early evaluation of right ventricular function is an important aspect of cardiogenic shock evaluation. Significant RV dysfunction portends poor prognosis, can necessitate more aggressive interventions, and defines the types of mechanical circulatory support necessary.
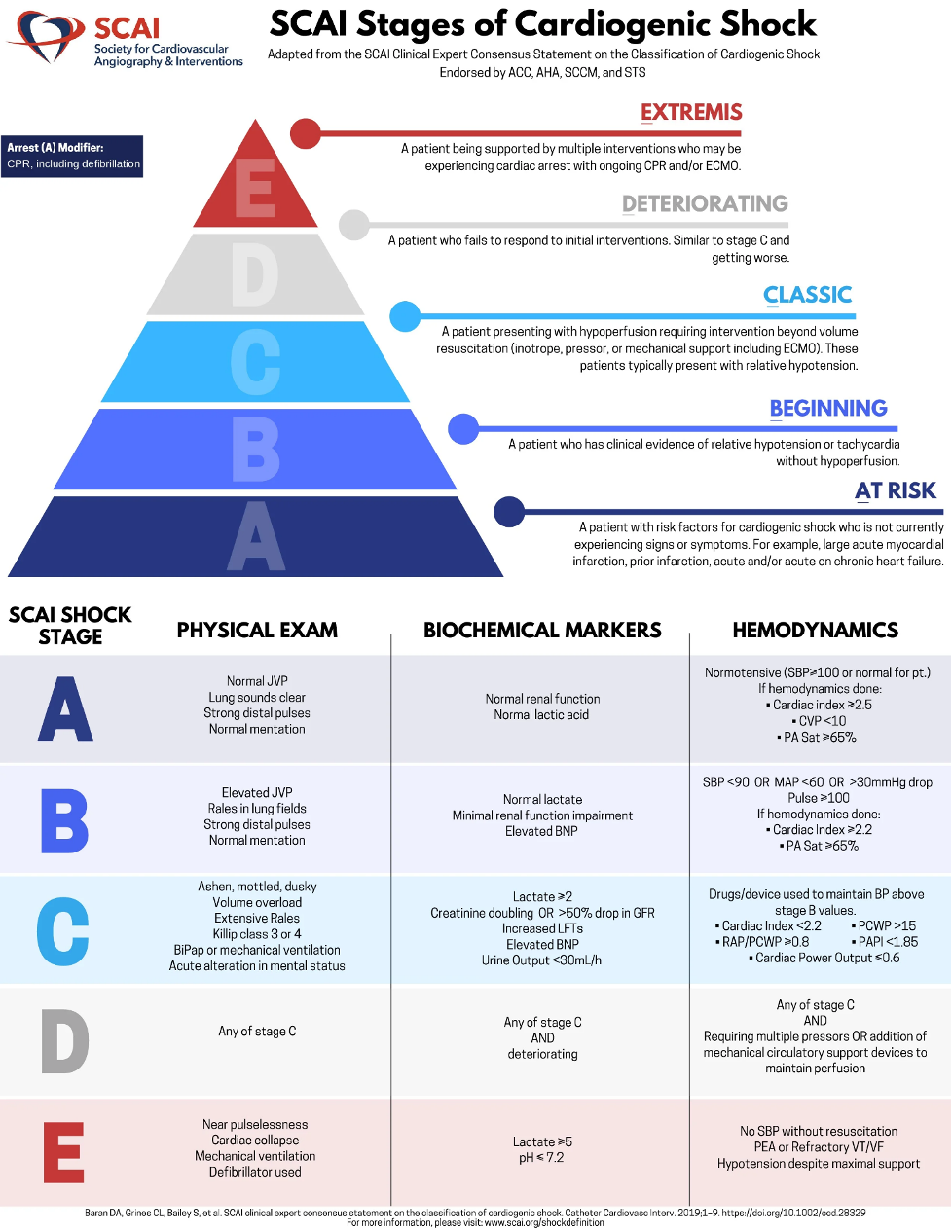
- Classification systems for cardiogenic shock help to further characterize a patient’s illness severity. The INTERMACS and SCAI classification systems are particularly designed to allow for early identification of patients who would most benefit from more advanced interventions such as vasoactive medications or mechanical circulatory support.
- Shock Team Calls improve mortality for patients in cardiogenic shock. By rapidly bringing together heart failure specialists, interventional cardiologists, cardiothoracic surgeons, and critical care physicians, appropriate interventions and contingencies can be discussed and quickly implemented without adding delays to patient care. Importantly, these calls should attempt to integrate patient goals of care in order to best serve our patients.
Show notes – Shock Team Call
1. What is the classic definition of cardiogenic shock?
- The classic definition of cardiogenic shock was initially derived from the Shock Trial published in 1999 (1). In this trial, cardiogenic shock was defined as shock due to left ventricular dysfunction occurring in the setting of acute myocardial infarction in the setting of acute MI as confirmed by specific criteria:
- Clinical criteria:
- SBP<90mmHg for at least 30 minutes
- Need for supportive measures to maintain SBP > 90mmHg
- End-organ hypoperfusion as defined by cool extremities, UOP <30ml/hr, HR > 60bpm
- Hemodynamic criteria:
- CI ≤ 2.2 L/min/m2 BSA
- PCWP ≥ 15mmHg
- Clinical criteria:
- With the advent of primary percutaneous coronary intervention, non-ischemic etiologies have become more prevalent as the etiology of cardiogenic shock such as decompensation of chronic heart failure, valvular heart disease, etc.
- As discussed on the episode, cardiogenic shock occurs on a spectrum from a “pre-shock” state to “extremis.” To facilitate early recognition of cardiogenic shock, appropriate phenotyping (e.g., LV-predominant, RV-predominant, biventricular, pericardial, valvular, pulmonary vascular, etc), timely interventions, and allocation of advanced therapies (e.g., mechanical circulatory support), a more granular approach to the classification is needed (see below regarding SCAI classification).
2. What are some of the clinical features of cardiogenic shock?
- Physical Exam Findings – A careful head-to-toe assessment should be conducted during the initial patient encounter. Important markers include (but are not limited to):
- Signs of hypervolemia
- Patient positioning as a sign of orthopnea
- Elevated JVP
- Tachypnea
- Presence of pulmonary rales
- Lower extremity edema
- Hepatomegaly
- Ascites
- Signs of poor organ perfusion
- Cool extremities
- Poor hourly urine output.
- Confusion or Altered Mental Status
- Signs of poor cardiac output
- Pulse quality – is it fast, slow, thready?
- Pulsus alternans – alternation between strong and weak beats in sinus rhythm without change in cadence or cycle length (a marker of low output and ejection from the LV) (2).
- Narrow pulse pressure
- Clues to help determine the etiology of the shock
- Point of maximal impulse displacement
- Right ventricular heave
- Auscultation of murmurs may indicate a valvular and/or congenital anomalies
- An accentuated P2 may indicate pulmonary hypertension
- Gallops may indicate filling pressures and/or underlying cardiomyopathy
- A pericardial knock may indicate constrictive pericarditis
- An irregular pulse may indicate an arrhythmia causing or contributing to shock
- Signs of hypervolemia
- Laboratory studies
- Laboratory markers of end organ hypoperfusion include markers of renal function such as creatinine and of hepatic injury (AST, ALT) and function (INR).
- Lactate has also been shown to display prognostic significance though clear correlations between objective thresholds to clinical outcomes have yet to be fully established.
- More important than individual values themselves are their temporal trends and the integration of multiple data points across numerous variables.
- Early Imaging studies
- EKG should be obtained and reviewed early after presentation to evaluate for acute coronary syndrome and need for urgent coronary angiography.
- Chest x-ray findings of pulmonary edema or effusions, assessment of heart size, and presence of cardiovascular hardware (sternal wires, implantable electrical devices, valvular interventions, etc).
- Focused transthoracic echocardiography, if available in the acute setting, can be helpful.
- Focused TTE should assess left and right ventricular morphology and function, the presence of a left ventricular thrombus, stenotic or regurgitant valvular lesions, or dynamic outflow tract obstructions.
- Echo surrogates of filling pressures may be supportive though may be limited by technique and image quality.
- Evaluation of RV function and illness severity
- Significant RV dysfunction is a marker of illness severity and leads to worse clinical outcomes.
- RV dysfunction limits total cardiac output, worsens systemic venous congestion, and worsens end organ dysfunction.
- RV assessment is critical when evaluating for the need for mechanical circulatory support, and severe RV dysfunction may increase the likelihood that MCS will be necessary.
- Severe RV dysfunction may necessitate the use of specific MCS devices (e.g., RV assist devices). It may also impact decision-making regarding what types of temporary or, even more importantly, durable MCS devices the patient may qualify for.
- Enjoy the upcoming RV-Predominant Shock Episode with Dr. Ryan Tedford for a more in-depth discussion!
- Invasive hemodynamic assessment
- Invasive hemodynamic evaluation with a pulmonary arterial catheter (PAC) is particularly useful for confirming and profiling cardiogenic shock as well as tailoring initial and subsequent management.
- An accurate assessment of filling pressures, cardiac output (by Thermodilution or Indirect Fick), right ventricular function, systemic vascular resistance, and specific calculated indices (e.g., CPO, PAPi, RA/PCWP) provide a more nuanced evaluation of a patient’s shock.
- Specifically, a PAC can assist in early identification of an under-recognized form of cardiogenic shock, under the classic Stevenson paradigm, a “wet and warm” picture. These patients have a systemic inflammatory response in addition to or as a result of their cardiac pathology, with a reduced cardiac index, low to normal SVR, and elevated pulmonary capillary pressures.
- Enjoy the upcoming Invasive Hemodynamics episode with Dr. Nosheen Reza and the following infographic from CardioNerds Academy Fellow, Dr. Ahmed Ghoneem, for more details!
3. How is cardiogenic shock classified and how are these classifications useful in the management of cardiogenic shock?
- Differentiating cardiogenic shock from other types of shock and the severity of shock can often be challenging. Constructs such as Dr. Lynne Warner Stevenson’s physical exam-based shock classifications are helpful in broadly phenotyping cardiogenic shock at the bedside (3). However, these classification systems may have their limitations. Determining the underlying etiology relies heavily on integrating various pieces of clinical information ranging from the physical exam as well as laboratory and imaging information. In clinical practice, the following classification systems and schemas are most used – Cardiogenic Shock Classification Systems:
- Killip Classification (4) – limited to acute myocardial infarction etiologies of cardiogenic shock:
- Class I – No evidence of heart failure
- Class II – Findings consistent with mild to moderate heart failure (e.g., S3 gallop, pulmonary rales less than one-half way up the posterior lung fields, or jugular venous distension)
- Class III – Overt pulmonary edema
- Class IV – Cardiogenic shock
- INTERMACS (5) – Provides more granularity to the illness severity by dividing NYHA Class III to IV heart failure patients into 7 distinct profiles:
- 1 – “Crash and Burn”: life-threatening hypotension refractory to intravenous inotropes, developed to understand patients who will require mechanical circulatory support (i.e., critical cardiogenic shock).
- 2 – “Sliding on inotropes”: worsening end-organ dysfunction despite use of intravenous inotropic medications.
- 3 – “Dependent stability”: stable hemodynamics and end-organ dysfunction but failure to wean from intravenous inotropes (i.e., inotrope-dependent)
- 4 – Resting symptoms, ambulatory NYHA IV: at home on oral therapy but with frequent symptoms of congestion at rest or with any activities of daily living
- 5 – Exertion intolerant: comfortable at rest but unable to engage in any activity, living predominantly within the house or housebound, but without overt congestion
- 6 – Exertion limited: comfortable at rest without evidence of fluid overload and able to do some mild activities of daily living, but gets fatigued within a few minutes of any meaningful exertion
- 7 – Advanced NYHA Class III: clinically stable with a reasonable level of comfortable activity, despite history of previous decompensation that is not recent
- SCAI Classification System (6 – see Figure) – specifically geared towards the classification of cardiogenic shock, defining disease severity, and following patients through their hospital stay
- A – At risk for cardiogenic shock
- B – Beginning of Cardiogenic Shock
- C – Classic Cardiogenic Shock
- D – Deteriorating
- E – Extremis
- Killip Classification (4) – limited to acute myocardial infarction etiologies of cardiogenic shock:
- Acute Ischemic Cardiogenic Shock vs Heart-Failure Cardiogenic Shock
- Understanding the underlying etiology of cardiogenic shock (e.g., acute ischemic vs. worsening chronic heart failure cardiogenic shock vs. acute heart failure cardiogenic shock) is very important in terms of management.
- The clinical trajectory (and often the hemodynamics) of acute MI shock is different from the trajectory of chronic heart failure derived cardiogenic shock. At the basic level, acute-MI shock is an abrupt event often affecting an otherwise potentially stable or ambulatory patient, and thus warrants consideration for revascularization. On the other hand, decompensation of chronic heart failure may necessitate consideration of advanced therapies such as temporary or durable mechanical circulatory support or heart transplantation.
4. What is a Shock Team and how do we prepare for a shock team call?
- Shock Team
- A shock team is designed to expeditiously bring together key members of the care team to determine patient management for a patient suspected to be in cardiogenic shock (7).
- These members often include the referring physician, advanced heart failure cardiologist, interventional cardiologist, and cardiothoracic surgeon. Cardiac intensivists, electrophysiologists, or cardiac anesthesiologists may also be included when appropriate. Each institution has their own policies regarding activation and composition of their teams.
- The Shock Team call allows for expedited discussions to 1) confirm the diagnosis and severity of cardiogenic shock and 2) determine next therapeutic steps along with contingencies.
- These discussions can include discussion of survival benefit, availability and type of interventions that can be offered, candidacy for advanced options, and patient values and preferences. Multiple studies have shown that these calls do not delay critical decision-making but in fact ensure appropriate level of support and allows for planning for care escalation. Shock teams have been shown to improve clinical outcomes for patients in cardiogenic shock (8).
- Preparing for a Shock Team Call
- The referring or presenting provider should include key clinical exam findings and objective laboratory or imaging data as outlined above.
- In addition to this, providers should strive to include information regarding who the patient is outside of the hospital. This can include their history within healthcare, the patient’s support system, and goals of care. Obtaining these details to whatever extent possible allows us to best serve our patients.
- Importantly, this information, along with consideration of the overall trajectory of the patient can be factored into decisions regarding appropriate interventions.
- The presenting provider may expect decisions that can range from initial stabilization on vasoactive medications to additional information needed from the cardiac catheterization laboratory to immediate plans for escalation to temporary or durable mechanical circulatory support.
Supplemental Images
References
Guest Profiles

Dr. Anu Lala-Trindade is an advanced heart failure and transplant specialist at Mount Sinai Hospital in New York City. She serves as the Director of Heart Failure Research and as Data Coordinating Center leadership for the NHLBI Cardiothoracic Surgery Network. A prolific educator, Dr. Lala has won numerous teaching awards and leads the fellowship program in Advanced Heart Failure and Transplant. A physician-scientist par excellence, she has authored numerous peer reviewed scientific publications and is the principal investigator for a number of clinical trials in heart failure. She serves as the deputy editor of the Journal of Cardiac Failure and also serves on local and national committees in the American Heart Association, American College of Cardiology, Heart Failure Society of America among others, devoted to advanced heart disease.

Dr. Mark Dela Cruz is currently an Advanced Heart Failure Fellow at the University of Chicago. Before then, he obtained his Bachelor of Arts degree at the University of Pennsylvania, where he graduated Summa Cum Laude with a double major in French Studies and with Distinction in Biological Basis of Behavior. He went on to obtain his medical degree and completed his internal medicine residency at the University of California, San Francisco where he participated in the clinical research pathway, Program in Residency Investigation Methods and Epidemiology. He served as a heart failure hospitalist before coming to the University of Chicago for Cardiology Fellowship. He has conducted research on vascular endothelium, and the interaction between HIV and Cardiology. Now, he focuses on translational research on the impact of the gut microbiome in heart transplantation. Born in Manila, Philippines, Dr Dela Cruz also maintains an interest in Filipino cardiovascular health and is an avid traveler.