
 Channel Your Enthusiasm
Channel Your Enthusiasm Chapter Two: Renal Circulation and Glomerular Filtration Rate, part 2
The exciting conclusion to Chapter Two: Renal Circulation and Glomerular Filtration Rate
- Determinants of GFR
- First step in making urine is separation of an ultrafiltrate
- Governed by starling forces
- Balance of hydraulic and osmotic forces
- GFR = LpS (P gc – P us - Osmotic Pressure Cap p)
- Normal GFR 95 in women, 120 in men
- Cap Hydrolic pressure remains constant
- glom cap Oncotic progressively rises
- Due to filtration of protein free fluid (protein concentration rises in the capillary)
- Filtration gradient begins at 13 mmHg and falls to zero after filtration of 20% or RPF!
- GFR is capped at 20% of RPF called filtration equilibrium
- So GFR is dependent on RPF, unless you can change glomerular hydraulic pressure
- Glomerular hydraulic pressure is controlled by balance of twin arteriole (afferent and efferent)
- Constriction of afferent arteriole reduces RPF, GFR, and glom pressure
- Dilation of afferent arteriole increases RPF, GFR, and glom pressure
- Constriction of the efferent arteriole increases Glom pressure, increasing GFR
- Besides glom hydrostatic pressure the other starlings forces are rarely relevant to changes in GFR
Letty says: referred to this NEJM review article later JC thought she was referring to something else -see #2- and then Roger referred to this again)
Normotensive Acute Renal Failure from Gary Abuelo in NEJM 2007. https://www.nejm.org/doi/10.1056/NEJMra064398 (note in this article, Dr. Abuelo acknowledges the newer terminology of the time, AKI rather than ARF but chooses not to embrace it). In figure 2, he highlights the classic examples of how autoregulation can be affected. In the table, additional examples are provided but all within the framework of alterations related to autoregulation and the interplay between the two resistance vessels.
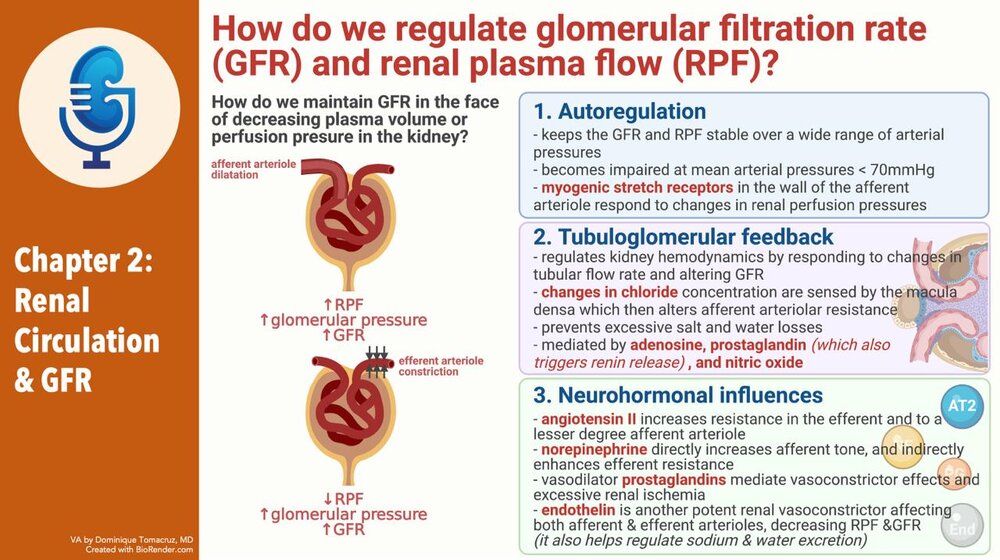
- Regulation of GFR
- Autoregulation
- The ability to keep glomerular pressure constant over wide range of systemic arterial pressure
- When pressure < 70 autoregulation fails and GFR will fall with decreases in systemic pressure
- When pressure falls below 40-50 GFR ceases
- At least some of this autoregulation is mediated with Ang2. Giving ACEi markedly disrupts autoregulation
- Nitric oxide, not important
- TGF

- Chloride in macula densa
- Blocked by furosemide
- Group affect of nephrons

- Ang 2 sensitizes
- Adenosine mediates
- Function of TGF
- 90% of filtrate is reabsobed in PT and LOH
- 10% is reabsobed dismally
- Need to control the amount of fluid delivered distally to prevent overwhelming the resorptive capacity of the distal nephron
- Talks about acute renal success without naming it (but did reference it)
- Mentions glucosuria blunts TGF. Hmmm...
- Neurohormonal influences

- Volume changes in ang2, sympathetic NS
- Role of PGE
- Interesting discussion of change of the nephrons perfumed with volume depletion, shifting of blood from outer coretex to inner medullary cortical gloms with their long loops
- Dopamine and ANP both increased with volume up
- Dopamine causes vasodilation of afferent and efferent arteriole
- ANP causes afferent vasodilation and efferent vasodilation constriction, increasing GFR without affecting RPF
- Glomerular hemodynamics and renal failure
- Decreased glomerular mass results in hyperfiltration of remaining gloms
- Mediated through afferent vasodilation
JC talks about this classic study in critical care: High vs. Low blood pressure target in Septic Shock. https://www.nejm.org/doi/pdf/10.1056/NEJMoa1312173
In this multi-center open label trial of 776 patients randomized to either a MAP of 65-70 or 80-85 with the primary endpoint of mortality. There was no difference in mortality at 28 days between the two groups (but a small difference in AKI in the patients who had chronic HTN- in the higher BP target, there was a decrease in need for RRT; there was also a higher incidence of afib in the high target group overall).
- Results in compensation and stable GFR in short term, long term maladaptive
- Reason for ACEi
- Clinical Evaluation of Renal Circulation
- Concept of clearance and measurement of GFR
- GFR as an index of functioning renal mass
- Had a patient today s/p nephrotomy, 72 years old, Cr0.9!
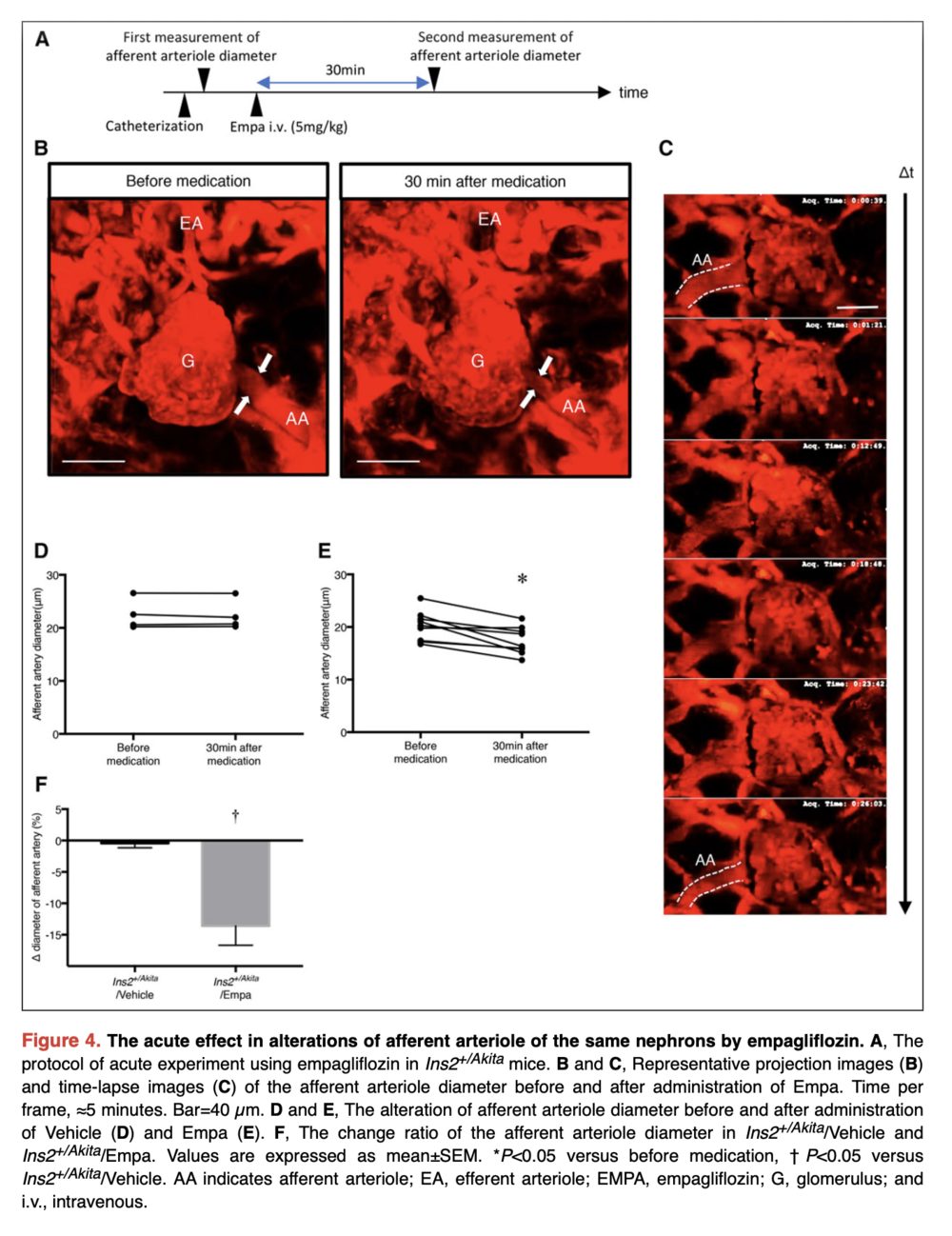
Melanie referred to this article in Circulation which demonstrates that SGLT2 inhibitors do decrease single nephron GFR (in mice) and that this is related to a decrease in the afferent arteriole diameter and then they show that this is related to a local increase in adenosine.
Kidokoro K, Cherney DZI et al. Evaluation of glomerular hemodynamic function by empagliflozin in diabetic mice using in vivo imaging Circulation 140 (4) 2019
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.118.037418
- Fall in GFR earlier and only sign of renal disease
- Serial monitoring is used to assess severity and follow the course of disease
- GFR is useful for dosing drugs
- How to measure GFR

- Consider fructose polysaccharide inulin (love the parenthetical, not insulin)
- Inulin filtered = inulin excreted
- Filtered inulin = plasma inulin concentration x GFR
- Inulin excreted = urine concentration x urine volume
- Use Alber a to get GFR = [Urine]insulin x urine volume / [plasma]inulin
- GFR = inulin clearance
- There is not an available assay for inulin
- Creatinine clearance
- Freely filtered
- Not reanbsorbed
- Not metabolized
- Small amount excreted
- CrCl exceeds GFR by 10-20%
Roger says the SGLT2 inhibitor story is about the afferent arteriole and he thought it reminded him of the MDRD study and the concept that the lower protein intake would be protective and delay the progression of CKD.
The concept was that low protein diets would decrease glomerular pressure by decreasing the intake of amino acids that lead to arteriolar vasodilation and increased GFR. Klaur S, Levey AS et al. The effects of Dietary Protein Restirciton and blood-pressure control on the progression of chronic renal disease. NEJM 1994 330:877-884.
https://www.nejm.org/doi/full/10.1056/nejm199403313301301
- Compensated for by noncreatinine chromogens (acetone proteins, as Orbi acid, pyruvate) that over estimate Cr by 10-20%
- Cr Cl = [Urine]cr x urine volume / [Plasma]cr
- Two major limitations
- Incomplete collections
- 20-25 mg/kg in adult men
- 15-20 mg/kg in adult women
The term “Acute renal success” comes from
Thurau K and Boylan JW. Acute renal success. The unexpected logic of oliguria in acute renal failure. Am J Med 1976 61(3): 3038-15.
- Falls by 50% from age 50 to 90 to 10 mg/kg
- Increased tubular secretion with decreased kidney function

- GFR of 40-80 cr secretion may account for as much as 35% of creatinine excretion
- In some cases CrCl can exceed GFR by a factor of 2
- Give cimetidine 1200 mg!
- It is important to appreciate however that exact knowledge of GFR is not required. More important to know if GFR is changing
- Why is radio labeling the solution DTPA and iothalamate?
- Talks about the reality of progressive disease despite stable GFR and CrCl
- On to plasma Cr and GFR
If you think placing dialysis lines is too easy, here is a wonderful review of micropuncture technique in the kidneys by Volker Vallon.
Micropuncturing the Nephron. Pflugers Arch 2009 458(1): 189-201. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2954491/
- Creatinine excretion = creatinine production (and this is constant)
- Creatinine excretion = [Cr] x GFR = constant
- If GFR falls in half, creatinine excretion will fall in half, while creatinine production remains the same, so creatinine will rise and rise until [Cr] x GFR = creatinine production and then it will level off.
- Changes in creatinine load
- High protein diet can increase it
- Vegetarian diet can decrease it
JC brought up studies on fenoldopam, of which there are many. This is one such study in patients undergoing cardiac surgery.
JAMA 2014 Bove T et al. Effect of fenoldopam on use of renal replacement therapy among patients with acute kidney injury after cardiac surgery: a randomized clinical trial https://pubmed.ncbi.nlm.nih.gov/25265449/
- Cooked meat can increase Cr by 1 mg/dL
- Talks about need for steady state to assess GFR
- Talks about the curvilinear relationship
- Then he talks Cockcroft Gault
The one, the only: The Cockcroft Gault:
Prediction of creatinine clearance from serum creatinine. Nephron 16: 31–41, 1976 https://pubmed.ncbi.nlm.nih.gov/1244564/
- Cirrhosis masks kidney insufficiency, low meat intake, low BUN production
- Can someone explain what we are supposed to take from figure 2-12
- Stable Cr does not mean stable kidney disease
Roger describes the study design for the seminal paper on the use of ACE inhibitors to slow the decline in renal function in diabetic kidney disease (then called diabetic nephropathy) and the decision to use the doubling of the serum creatinine as an endpoint.
Lewis EJ The effect of Angiotensin-converting-enzyme inhibition on diabetic nephropathy NEJM 1993 https://www.nejm.org/doi/full/10.1056/NEJM199311113292004
- Ketoacidosis can raise the Cr 0.5 to 2.0mg/dL
- On to BUN
- Destination of amino acids produces ammonia
- We detoxify ammonia by converting to urea
- Increased with increased protein load
- Increased catabolism
Melanie mentioned an old study on ingestion of expired blood: Cohen TD. Induced azotemia in humans following massive protein and blood ingestion and the mechanism of azotemia in gastrointestinal hemorrhage.
AM J Med Sci 1956 https://pubmed.ncbi.nlm.nih.gov/13302213/
- Tetracycline causes decreased anabolism
- Trauma
- Steroids
- Urea excretion is variable and tied to hydration and FF
- Renal plasma flow and PAH
