
 Cardionerds: A Cardiology Podcast
Cardionerds: A Cardiology Podcast 417. Case Report: Clear Vision, Clouded Heart: Ocular Venous Air Embolism with Pulmonary Air Embolism, RV Failure, and Cardiac Arrest – Trinity Health Ann Arbor
Managing Air Embolism
- Stop further air entry immediately if air embolism is suspected.
- Administer 100% oxygen promptly to improve tissue oxygenation and accelerate nitrogen washout.
RV Physiology and Failure
- The right ventricle (RV) tolerates volume changes well but poorly handles sudden pressure increases.
- RV dilation impairs contractility, causes functional tricuspid regurgitation, and hinders left ventricular filling via interventricular dependence.
Support Strategies for RV Failure
- Optimize right ventricular preload carefully to avoid worsening venous congestion.
- Use inotropes like dobutamine to boost RV contractility and consider norepinephrine for blood pressure support.
CardioNerds Critical Care Cardiology Council members Dr. Gurleen Kaur and Dr. Katie Vanchiere meet with Dr. Yash Patel, Dr. Akanksha, and Dr. Mohammed El Nayir from Trinity Health Ann Arbor. They discuss a case of pulmonary air embolism, RV failure, and cardiac arrest secondary to an ocular venous air embolism. Expert insights provided by Dr. Tanmay Swadia. Audio editing by CardioNerds Academy intern, Grace Qiu.

A 36-year-old man with a history of multiple ocular surgeries, including a complex retinal detachment repair, suffered a post-vitrectomy collapse at home. He was found hypoxic, tachycardic, and hypotensive, later diagnosed with a pulmonary embolism from ocular venous air embolism leading to severe right heart failure. Despite a mild embolic burden, the cardiovascular response was profound, requiring advanced hemodynamic support, including an Impella RP device (Abiomed, Inc.). Multidisciplinary management, including fluid optimization, vasopressors and mechanical support to facilitate recovery. This case underscores the need for early recognition and individualized intervention in cases of ocular venous air embolism.
“To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all.” – Sir William Osler. CardioNerds thank the patients and their loved ones whose stories teach us the Art of Medicine and support our Mission to Democratize Cardiovascular Medicine.
US Cardiology Review is now the official journal of CardioNerds! Submit your manuscript here.
Pearls- Clear Vision, Clouded Heart: Ocular Venous Air Embolism with Pulmonary Air Embolism, RV Failure, and Cardiac Arrest
- Hypoxia, hypotension and tachycardia in a patient following ocular instrumentation are classic findings suggestive of pulmonary embolism from possible air embolism.
- The diagnosis of RV failure is based on clinical presentation, echocardiographic findings (such as McConnell’s sign), and invasive hemodynamic assessment via right heart catheterization.
- Mechanical circulatory support can be considered as a temporary measure for patients with refractory RV failure.

Notes – Clear Vision, Clouded Heart: Ocular Venous Air Embolism with Pulmonary Air Embolism, RV Failure, and Cardiac Arrest
1. What is an Ocular Venous Air Embolism (VAE), and how can it be managed in critically ill patients?
- An Ocular Venous Air Embolism is defined as the entry of air into the systemic venous circulation through the ocular venous circulation, often during vitrectomy procedures. Early diagnosis is key to preventing cardiovascular collapse in cases of Ocular Venous Air Embolism (VAE).
- The goal is to stop further air entry. This can be done by covering the surgical site with saline-soaked dressings and checking for air entry points.
- Adjusting the operating table can help, especially with a reverse Trendelenburg position for lower-body procedures.
- The moment VAE is suspected, discontinue nitrous oxide and switch to 100% oxygen. This helps with oxygenation, speeds up nitrogen elimination, and shrinks air bubbles.
- Hyperbaric Oxygen Therapy can reduce bubble size and improve oxygenation, especially in cases of cerebral air embolism, when administered within 6 hours of the incident.
- Though delayed hyperbaric oxygen therapy can still offer benefits, the evidence is mixed.
- VAE increases right heart strain, so inotropic agents like dobutamine can help boost cardiac output, while norepinephrine supports ventricular function and systemic vascular resistance, but this may also worsen pulmonary resistance.
- Aspiration of air via multi-orifice or Swan-Ganz catheters has limited success, with success rates ranging from 6% to 16%. In contrast, the Bunegin-Albin catheter has shown more promise, with a 30-60% success rate. Catheterization for acute VAE-induced hemodynamic compromise is controversial, and there’s insufficient evidence to support its widespread emergency use.
2. What are the key hemodynamic parameters used to assess RV function?
- On echocardiogram, there are a number of parameters that can assess RV function:
- Tricuspid Annular Plane Systolic Excursion (TAPSE): Measures the lateral tricuspid annulus’ movement during systole. A TAPSE value below 1.6 cm is associated with poor prognosis.
- RV Outflow Tract (RVOT) Acceleration Time: Measured via pulsed wave Doppler, an acceleration time of <100 ms is abnormal, with values ≤60 ms indicating a worse prognosis.
- Global RV Longitudinal Strain: Assessed via speckle tracking, with a strain value of −20% being highly predictive of RV dysfunction (normal values typically range -24.5 to -28.5%).
- Tricuspid Regurgitation (TR) Jet Velocity: Helps estimate pulmonary systolic pressure and provides prognostic information.
- Inferior Vena Cava (IVC) Collapsibility: Useful in estimating right atrial pressure and guiding volume resuscitation, though it lacks prognostic significance.
- The RV:LV diameter ratio offers prognostic value, with a ratio greater than 0.9 linked to worse outcomes.
- Invasive Hemodynamic Monitoring (Right heart catheterization, PA Catheter)
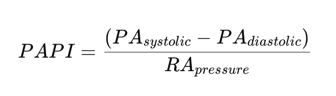
- The Pulmonary Artery Pulsatility Index (PAPI) is an invasive hemodynamic parameter used to assess right ventricular (RV) function, particularly in cases of RV failure and cardiogenic shock. PAPi is the pulmonary arterial pulse pressure divided by the RA pressure. A PAPi of <0.9 is a poor indicator, especially in the acute myocardial infarction population.
3. What are the core principles in managing a patient with RV failure?
- The management to optimize RV function is centered around optimizing preload, afterload, and contractility.
- Optimizing preload – Optimizing preload is one of the most important aspects in the management of acute decompensated RV failure. The majority of us are taught that the RV is “preload dependent” and patients should be fluid resuscitated. However, many patients are actually volume overloaded and may benefit from diuresis. Overall, this is a patient-to-patient decision, depending on the clinical picture, to optimize preload; though the use of pulmonary artery (PA) catheters in this setting is not well supported.
- Reducing afterload – Avoid intubation if clinically feasible, as they may increase PVR; however, if essential, ideally, oxygen saturation (SaO₂) should be maintained above 92%, and ventilator settings should be adjusted to optimize lung volume and maintain a normal pH and PCO₂. Nitric oxide has also been beneficial in improving oxygenation and reducing PVR with its vasodilatory effects.
- Support cardiac output
- May support with the use of inotropes as well as mechanical circulatory support.
- Pressors: The ideal vasopressor increases systemic arterial pressure and RV contractility without raising pulmonary vascular resistance.
- Norepinephrine: Primarily an α1 agonist, it improves systemic blood pressure with some β1 stimulation. It has shown benefits in maintaining RV-PA coupling.
- Dobutamine: A β1 agonist that improves myocardial contractility and RV-PA coupling, though it can cause vasodilation at higher doses.
- In general, dobutamine is considered the best for acute RVF with PH, unless hypotension is a significant concern, in which case norepinephrine might be preferred. Milrinone is another option.
- MCS: short-term MCS should be considered in patients with cardiogenic shock as a bridge to recovery, a bridge to decision, or a bridge to bridge whilst the underlying causes for cardiogenic shock are addressed further described below
- Options include:
- Venous-arterial extracorporeal membranous oxygenation (V-A ECMO)
- RA to PA extracorporeal pump. (surgical RVAD)
- Flow device with an intake in the RA and an output in the PA. (Impella RP, Protek Duo)
- Options include:
- Pressors: The ideal vasopressor increases systemic arterial pressure and RV contractility without raising pulmonary vascular resistance.
- May support with the use of inotropes as well as mechanical circulatory support.
4. When should we consider mechanical circulatory support for right ventricular (RV) failure?
- Short-term MCS should be considered in patients with cardiogenic shock as a bridge to recovery, a bridge to decision, or a bridge to bridge whilst the underlying causes for cardiogenic shock are addressed.
- Clinical parameters that suggest acute MCS use include signs of relative hypoperfusion plus hemodynamic features suggestive of RV failure, which were present in our patient. A specific additional consideration relates to where acute left-sided MCS reveals acute RV failure. Discerning whether this is intrinsic RV failure or due to persistently elevated RV afterload from inadequate LV support is also essential, as it will define management.
- The goal of percutaneous mechanical support is to bypass the right ventricle and improve hemodynamics, while allowing time for optimization of the patient and recovery of the RV.
References
Arrigo, Mattia, et al. “Diagnosis and Treatment of Right Ventricular Failure Secondary to Acutely Increased Right Ventricular Afterload (Acute Cor Pulmonale). A Clinical Consensus Statement of the Association for Acute CardioVascular Care (ACVC) of the ESC.” European Heart Journal. Acute Cardiovascular Care, vol. 13, no. 3, 22 Dec. 2023, pp. 304–312, https://doi.org/10.1093/ehjacc/zuad157. Accessed 17 May 2024.
Chen, Guohai, et al. “INCIDENCE of ENDOPHTHALMITIS after VITRECTOMY: A Systematic Review and Meta-Analysis.” Retina (Philadelphia, Pa.), vol. 39, no. 5, May 2019, pp. 844–852, pubmed.ncbi.nlm.nih.gov/29370034/, https://doi.org/10.1097/IAE.0000000000002055.
Fakkert, Raoul A, et al. “Early Hyperbaric Oxygen Therapy Is Associated with Favorable Outcome in Patients with Iatrogenic Cerebral Arterial Gas Embolism: Systematic Review and Individual Patient Data Meta-Analysis of Observational Studies.” Critical Care, vol. 27, no. 1, 12 July 2023, https://doi.org/10.1186/s13054-023-04563-x. Accessed 7 June 2024.
Flaxel, Christina J., et al. “Idiopathic Epiretinal Membrane and Vitreomacular Traction Preferred Practice Pattern®.” Ophthalmology, vol. 127, no. 2, Feb. 2020, pp. P145–P183, https://doi.org/10.1016/j.ophtha.2019.09.022. Accessed 16 July 2020.
Frémont, Benoît, et al. “Prognostic Value of Echocardiographic Right/Left Ventricular End-Diastolic Diameter Ratio in Patients with Acute Pulmonary Embolism.” Chest, vol. 133, no. 2, Feb. 2008, pp. 358–362, https://doi.org/10.1378/chest.07-1231.
Huang, Ryan S, et al. “Pars Plana Vitrectomy with Silicone Oil or Gas Tamponade for Uncomplicated Retinal Detachment: A Systematic Review and Meta-Analysis.” American Journal of Ophthalmology, vol. 266, Oct. 2024, pp. 144–155, pubmed.ncbi.nlm.nih.gov/38815844/, https://doi.org/10.1016/j.ajo.2024.05.008.
Kanwar, Manreet K, et al. “Epidemiology and Management of Right Ventricular-Predominant Heart Failure and Shock in the Cardiac Intensive Care Unit.” European Heart Journal. Acute Cardiovascular Care, vol. 11, no. 7, 29 June 2022, pp. 584–594, https://doi.org/10.1093/ehjacc/zuac063. Accessed 5 Mar. 2023.
Lahm, Tim, et al. “Medical and Surgical Treatment of Acute Right Ventricular Failure.” Journal of the American College of Cardiology, vol. 56, no. 18, Oct. 2010, pp. 1435–1446, www.onlinejacc.org/content/56/18/1435, https://doi.org/10.1016/j.jacc.2010.05.046. Accessed 30 Nov. 2019.
Mirski, Marek A., et al. “Diagnosis and Treatment of Vascular Air Embolism.” Anesthesiology, vol. 106, no. 1, 1 Jan. 2007, pp. 164–177, pubs.asahq.org/anesthesiology/article/106/1/164/8884/Diagnosis-and-Treatment-of-Vascular-Air-Embolism, https://doi.org/10.1097/00000542-200701000-00026. Accessed 13 Apr. 2021.
Moon, Young Eun. “Venous Air Embolism during Vitrectomy: A Rare but Potentially Fatal Complication.” Korean Journal of Anesthesiology, vol. 67, no. 5, 1 Jan. 2014, pp. 297–297, pmc.ncbi.nlm.nih.gov/articles/PMC4252339/, https://doi.org/10.4097/kjae.2014.67.5.297. Accessed 10 Mar. 2025.
“Right Ventricular Failure.” Escardio.org, 2016, www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-14/Right-ventricular-failure.
Stickel, Simone, et al. “The Practical Management of Fluid Retention in Adults with Right Heart Failure due to Pulmonary Arterial Hypertension.” European Heart Journal Supplements, vol. 21, 1 Dec. 2019, pp. 46–53, academic.oup.com/eurheartjsupp/article/21/Supplement_K/K46/5678698, https://doi.org/10.1093/eurheartj/suz207.
Ventetuolo, Corey E., and James R. Klinger. “Management of Acute Right Ventricular Failure in the Intensive Care Unit.” Annals of the American Thoracic Society, vol. 11, no. 5, 1 June 2014, pp. 811–822, www.ncbi.nlm.nih.gov/pmc/articles/PMC4225807/#:~:text=Abstract, https://doi.org/10.1513/AnnalsATS.201312-446FR. Accessed 10 Aug. 2020.
What Is Vitrectomy. “What Is Vitrectomy?” American Academy of Ophthalmology, 15 May 2019, www.aao.org/eye-health/treatments/what-is-vitrectomy.
Zhao, Steven, and Oren Friedman. “Management of Right Ventricular Failure in Pulmonary Embolism.” Critical Care Clinics, vol. 36, no. 3, July 2020, pp. 505–515, https://doi.org/10.1016/j.ccc.2020.02.006. Accessed 29 Nov. 2020.
239. CCC: Approach to RV Predominant Cardiogenic Shock with Dr. Ryan Tedford
