Show Notes
-
General
-
Pain in joint for pediatric patient has a broad differential, including transient synovitis and septic arthritis
-
Transient synovitis, also known as toxic synovitis, is a common condition affecting kids aged 3-10 and often occurs after a viral infection. It is typically self-limiting and not considered a serious condition.
-
Septic arthritis is an infection in the joint space, typically affecting only one joint. It is often difficult to diagnose due to the fact that many patients, particularly under the age of 3, may not be able to localize their pain to a specific joint.
-
Workup
-
Diagnostic work-up for septic arthritis begins with blood work, which includes a complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and blood cultures. Lyme disease studies may also be necessary since Lyme disease can cause joint pain.
-
Patients with transient synovitis typically have mild elevation in inflammatory markers, while those with septic arthritis usually show a significant elevation.
-
Imaging studies, including X-rays, ultrasound to evaluate for a joint effusion, and MRI to assess for associated osteomyelitis, are also part of the diagnostic approach.
-
The Kocher criteria, developed specifically for septic arthritis of the hip, are a useful tool for clinical decision-making. The criteria include fever above 38.5 C, inability to bear weight, ESR above 40, and a white blood cell count above 12,000.
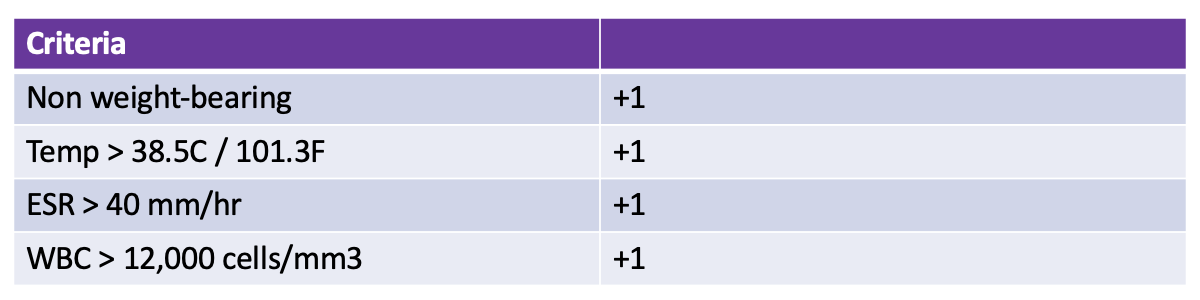
1 criterion met = 3% probability of septic arthritis
2 criteria met = 40% probability of septic arthritis
3 criteria met = 93% probability of septic arthritis
4 criteria met = 99+% probability of septic arthritis
-
If septic arthritis is suspected, orthopedics should be consulted immediately. Joint fluid aspiration is necessary for diagnosis and should not be delayed. The fluid should be sent for cell count, gram stain, glucose, culture, and PCR if available.
-
Septic arthritis is most commonly caused by bacterial infections, with Staph aureus being the most common organism. In school-age children, other bacteria such as Strep pyogenes, Strep pneumoniae, and Haemophilus influenzae should also be considered. In preschool-aged children, K. kingae is also considered. In older children and neonates, the range of potential bacteria varies.
-
Management
-
Empiric antibiotic therapy should target the most likely organisms and should not be delayed. Antibiotics may be narrowed once culture results are obtained.
-
The choice of antibiotics is dependent on the age group, with specific combinations suggested for neonates, children between 1 month and 4 years, and children aged 5 and older.
-
Cultures are only positive in 50-60% of cases. Synovial fluid PCR studies can help narrow antibiotic treatment.
-
Take Home Points
-
Limp in the pediatric population can commonly be transient synovitis but we should always consider septic arthritis
-
Some clues in the history and physical that would point you towards septic arthritis include fever, refusal to bear weight, and limited range of motion on exam
-
We are going to have to get labs, including CBC, inflammatory markers, and preoperative labs, along with an XR and possibly an ultrasound
-
Kocher criteria is one tool that can help us determine if this is a patient that requires a joint tap.
-
Arthrocentesis is the gold standard for diagnosis, but antibiotics should be started promptly if the diagnosis is suspected.
-
The choice of antibiotics is dependent upon age group.
-
Always cross check with institutional preferences / guidelines when choosing antibiotics

 Core EM - Emergency Medicine Podcast
Core EM - Emergency Medicine Podcast