Cardionerds: A Cardiology Podcast
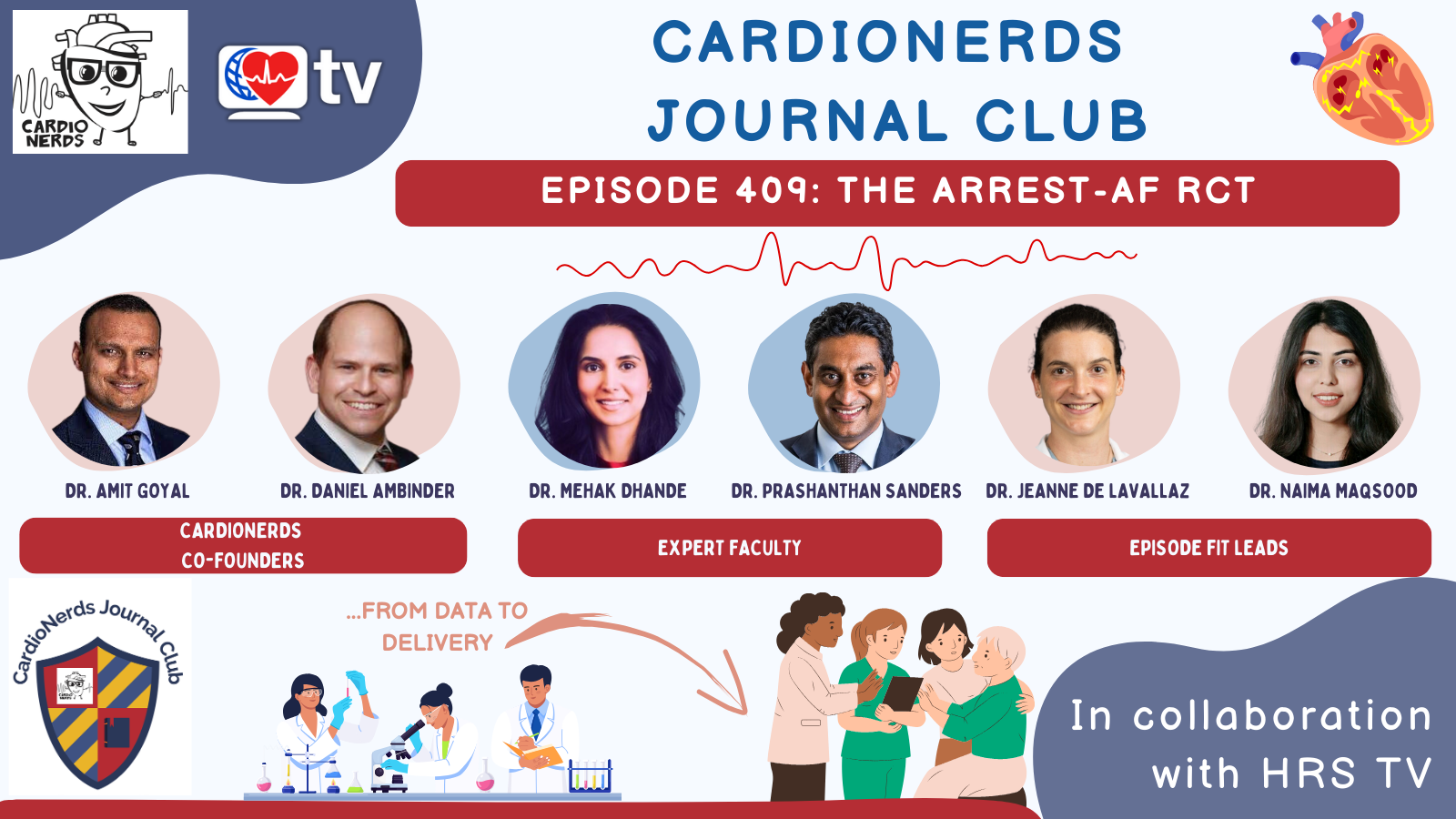
Cardionerds: A Cardiology Podcast 409. Journal Club: The ARREST-AF Trial with Drs. Prashanthan Sanders and Mehak Dhande
7 snips
Jan 31, 2025 Dr. Prashanthan Sanders, a leader in atrial fibrillation prevention, and Dr. Mehak Dhande, an electrophysiologist focusing on lifestyle changes, discuss the groundbreaking ARREST-AF trial. They reveal how an intensive risk factor management program significantly improved outcomes for atrial fibrillation patients. Topics include successful lifestyle modifications like weight loss and better management of health conditions, along with strategies to enhance patient education and access to care. Their insights emphasize the need for tailored approaches in cardiovascular health.
AI Snips
Chapters
Transcript
Episode notes
AFib Management
- Prioritize rate control for symptomatic relief in AFib patients.
- Then consider rhythm control and always address anticoagulation needs.
Combined Treatment
- Lifestyle changes aren't separate from other treatments, but boost them.
- Prior studies already hinted at this before ARREST-AF's randomized data.
Concurrent Management
- Offer rhythm control and lifestyle changes concurrently for AFib.
- Don't treat lifestyle and ablation as sequential steps.