
 Protrusive Dental Podcast
Protrusive Dental Podcast Cracked Teeth Clinical Guidelines – Chase? Fibers? WHEN to Intervene – PDP246
Cracked teeth — the diagnosis we all hate as Dentists!
How do you decide when to monitor and when to intervene?
What is the recommended intervention at different scenarios of cracks?
Should we be chasing cracks and reinforcing with fibers; is there actually enough long-term data to support that approach?
Over the years, we’ve had some epic episodes on this topic — from Kreena Patel’s “I Hate Cracked Teeth” (PDP028) to Dr. Lane Ochi’s Masterclass on Diagnosis and Management (PDP175).
But in this brand-new episode, Jaz is joined by Dr. Masoud Hassanzadeh to bring it all together — not just the diagnosis of cracks, but their management. They explore when to intervene, the role of fibers in preventing propagation, and even the fascinating possibility that cracks in teeth may have some ability to heal, just like bone!
This one’s a deep dive that will change how you talk to patients — and how you approach cracked teeth in your own practice.
Protrusive Dental Pearl
Your patient’s history predicts the future!
- Ask if past extractions were difficult → clues you into anatomical challenges.
- Ask how they lost other teeth → if cracks, be proactive with today’s cracks.
History isn’t just background—it’s a clinical tool.
Need to Read it? Check out the Full Episode Transcript below!
Key Takeaways
- Cracks in teeth can be diagnosed using magnification and high-quality imaging.
- Patient factors such as age and muscle strength play a significant role in crack prognosis.
- Symptomatic cracks should be treated to prevent further propagation.
- Understanding the anatomy of the tooth is crucial for effective treatment.
- The healing mechanism of cracks in teeth is possible but varies between enamel and dentin.
- Fibers can be used to strengthen restorations and manage cracks effectively.
- Long-term studies are needed to assess the effectiveness of current crack management protocols.
- The use of fluorescence filters can help identify bacteria in cracks.
- Chasing cracks should be done cautiously to avoid pulp exposure.
- A comprehensive understanding of crack mechanics can improve treatment outcomes.
Highlights of this episode:
- 00:00 Teaser
- 00:47 Intro
- 03:08 Protrusive Dental Pearl – The Importance of Dental History
- 07:18 Interview with Masoud Hassanzadeh
- 08:22 Diagnosing and Managing Cracks
- 21:13 When to Intervene on Cracks
- 25:50 Restoration Techniques and Materials
- 28:30 Chasing Cracks: Guidelines and Techniques
- 36:50 Mechanisms of Crack Healing in Teeth
- 45:11 Exploring the Use of Fibers in Dentistry
- 52:43 Introducing the Book on Cracked Teeth
- 54:57 Percussion-Based Diagnostics (QPD)
- 56:44 Key Takeaways
- 57:21 Conclusion and Final Thoughts
- 01:00:07 Outro
As promised, here are the studies mentioned during the discussion:
- Why cracks do not propagate as quickly in root dentin: Study 1a & 1b
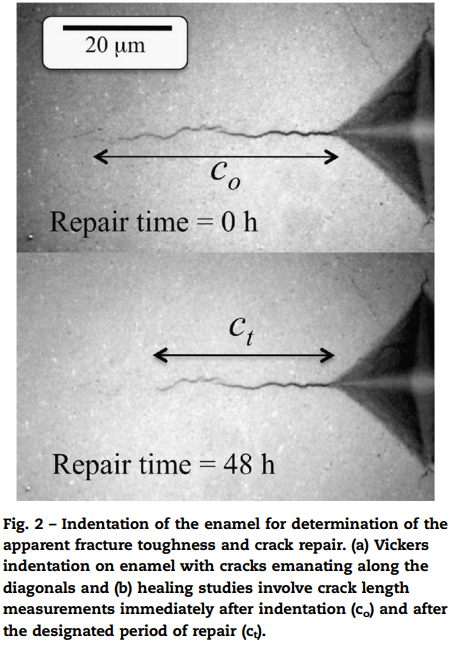
Root dentin has significantly higher fracture toughness compared to coronal dentin—nearly twice as tough, as demonstrated in multiple studies. The key difference lies in their structure and toughness. Root dentin’s unique collagen orientation adds strength, while its fewer lumens and thinner peritubular cuffs make it less brittle. In contrast, coronal dentin has thicker cuffs, which increase brittleness. Unlike coronal dentin, which fractures uniformly, radicular dentin is anisotropic—its fracture behavior varies depending on direction. These structural features give root dentin greater resistance to cracking, making it more durable under stress. - Studies on decreasing crack length due to crack repair in enamel. Study 2
- The importance of the modulus of elasticity of the final restoration in arresting crack propagation. Study 3
Historical Studies on Enamel Crack Healing
– 1949 (Sognnaes): The Organic Elements of the Enamel: III. The Pattern of the Organic Framework in the Region of the Neonatal and other Incremental Lines of the Enamel
– 1994 (Hayashi): High Resolution Electron Microscopy of a Small Crack at the Superficial Layer of Enamel
– 2009 (S. Myoung): Morphology and fracture of enamel
Don’t miss out — get instant access to all the research papers discussed here at protrusive.co.uk/cracks!
Dr. Masoud Hassanzadeh has written two essential books every dentist should own:
📘 Glossary of Biomimetic Restorative Dentistry
🔑 Your quick-reference guide to the language and principles of biomimetics — explained in a way you can actually use chairside.
📕 The Cracked Tooth: A Comprehensive Guide to Cracked Teeth
🦷 Everything you need to know about diagnosis, management, and the science behind one of dentistry’s biggest headaches.
🌴✨ Dubai 2026: Occlusion + Family Fun ✨🌴
This Easter, join Dr. Jaz Gulati and Dr. Mahmoud Ibrahim for something truly special — a tax-efficient holiday that mixes world-class occlusion training with plenty of family time in Dubai.
🦷 What’s included?
⏰ 20 hours of hands-on occlusion (mornings only: 9 am–1 pm)
🏖️ Afternoons & evenings free to enjoy Dubai with your family
📚 Pre-learning + online content to deepen your understanding
🥂 A not-for-profit event — just dentists, families, and fun!
👉 Learn more & get your quote at: globaldentalevents.co.uk
💡 Make memories with your loved ones while making your CPD hours tax-deductible
Want to level up your knowledge on cracked teeth? 🎧 Don’t miss PDP098: Cracked Teeth Management with the Direct Composite Splint Technique
#PDPMainEpisodes #EndoRestorative #BreadandButterDentistry
This episode is eligible for 1 CE credit via the quiz on Protrusive Guidance.
This episode meets GDC Outcomes A and C.
AGD Subject Code: 070 ENDODONTICS
Aim: To provide clinicians with practical, evidence-based guidance for diagnosing, monitoring, and restoring cracked teeth, with emphasis on prognosis, risk factors, and restorative decision-making.
Dentists will be able to –
- Differentiate between enamel and dentine cracks, and recognize when prognosis is hopeless.
- Apply appropriate diagnostic tools and clinical criteria to decide when to monitor versus intervene.
- Select suitable restorative strategies and materials to manage cracked teeth effectively.
Click below for full episode transcript:
Teaser: After 48 hours, they started to see that the crack is just decreasing, like it's just healing. Is it really possible? But it is possible. Like how there is a crack healing mechanism in the bone, there is also crack healing mechanism in the tooth. When I started to learn about cracks, actually the studies were not from dentists.
Teaser:
They were fracture mechanic engineering that they just studied about the crack, and nowadays there is a new system, it is called quantitative percussion diagnostic, QPD. There is a stress concentration in that point where the crack is started, so we have to distribute the stress in that place, in that plane. That is the important one. If we are just going to remove the crack and put the restoration on it, I’m afraid it’s just going to happen again.
Jaz’s Introduction:
Over the years, we’ve had some awesome episodes on cracked teeth. If you go all the way back to PDP028 with Krina Patel, the episode was titled, I Hate Cracked Teeth, and you know what? I still hate cracked teeth. They’re a damn nuisance. They’re everywhere, and it creates major consent and if the tooth goes non-vital, that kind of conversation, which no one likes.
Now, years later, we did this epic episode with Dr. Lane Ochi, PDP175. You need to check these two episodes out if you want to geek out on cracks. But you know what? This episode really does a wonderful summary of cracks. Not just the diagnosis, but the actual management. Should we be chasing cracks? Are fibers actually indicated? Is there enough long-term clinical data to support the use of fibers in crack propagation? And the question of, okay, when should you actually intervene?
And you know what? The most important one I haven’t even mentioned yet. So, Dr. Masoud, the way I got acquainted with him is on social media. I posted this image of a crack, a really nasty crack, and he said something absolutely ridiculous. He said that cracks have an ability to heal a bit like cracks heal in bone.
Now, you said that because in this image I posted on social media, it was all about how I communicate cracks to my patients. I say to them, look, when you have a crack in a bone, the bone can heal, it can regenerate, but a crack in a tooth can never heal. Patients seem to resonate and they understand that. But he was suggesting that actually cracks can heal naturally a bit like bone. And so if you listen to the end of the podcast, you will see how that is actually possible.
Hello, Protruserati. I’m Jaz Gulati and welcome back to your favorite dental podcast. I’ve had a month in August which was pretty crazy. I didn’t do much recording of new podcasts. We were working on some of the older recordings I had done. We’ve got a huge backlog as a team, which is a wonderful position to be. We are having so much fun creating these episodes. Thank you to everyone who returns to our podcast, and of course all the new people that find us.
If you’re not already, you need to join 5,000 of the nicest and geekiest dentists in the world on the Protrusive Guidance app. Go on protrusive.app, make an account. Your only requirement is you must be nice and you must be geeky. If you are those two things, you should come and join us to geek out, discuss, share challenges, share wins. It’s a nice wholesome environment we’ve created far, far, far away from the toxicity you get on Facebook.
Dental Pearl
Now in true PDP fashion, I’m gonna give you a Protrusive Dental Pearl. This pearl helps me when I’m decision-making with my patients, and it’s all about probing further into the history of the patient. What I mean by that is when we have that patient, and we’re planning an extraction, let’s say the tooth has had it, it needs to come out, and we’re trying to gauge, will this be a difficult extraction or not? Did you know asking them if their previous extractions were difficult is actually a useful indicator? An oral surgeon once taught me this, and I think it’s true.
People have certain features that make their teeth more difficult to remove, certain curves, certain densities of bone, and that’s a useful thing to have in your history. Now, similarly in cracked tooth management, it’s good to ask a patient how they lost their other teeth. So if you see a patient and they’ve lost some molars and premolars, you should ask, well, how did this happen? For what reason did you lose the teeth?
If they mention cracks as the reason why they lost those teeth, those other cracks which are asymptomatic, because 90% of cracks are asymptomatic, now you have a reason to be a bit more proactive and less of the wait-and-watch and more of the, well, let’s prevent this from happening to any other teeth. Those are two clear examples of how the patient’s history, i.e. the complexity of the extraction and the reason for tooth loss being cracks, are useful in decision-making for the patient going forward.
Now, I’m actually very excited to get to the main episode. Honestly, this is such a beautiful, geeky episode with real tangible clinical nuggets for you to take away. And before we start this episode, I just wanna give a quick plug to our trip in Dubai 2026. So Easter holidays 2026, we’ve got UK dentists and their families and some Aussie dentists who are gonna go to Dubai to learn occlusion with me and Mahmoud. Why are we doing this? It’s Easter holiday, it’s Easter vacation. I wanna take my kids and my wife. We want to have some family fun in Dubai, but we want it to be tax deductible.
So how are we doing that? Picture this for those of us with families and kids. Bring everyone along. We’re gonna make it a very tax efficient holiday for you. We’ll be learning occlusion from 9:00 AM to 1:00 PM for the five days. So that’s 20 hours of hands-on occlusion, and the rest of the day is self-study. Go to the pool, have some cocktails while you think about occlusion. Go enjoy the nightlife of Dubai while thinking about occlusion, of course. You get to enjoy most of the day with your family or with your friends in Dubai, and it’s just the morning part where we’ll do the education.
You also get access to a lot of online content and pre-learning, and we actually genuinely want you to come out having learned occlusion to a very high standard. But actually, I’ll be honest with you, this is about the education, but it’s also about having a good time in a tax deductible or tax efficient way.
So if that’s piqued your interest, I want you to go to globaldentalevents.co.uk. That’s globaldentalevents.co.uk. Like I said, you don’t have to be from the UK to come to this. We’ve got some interest in Scandinavia. We’ve got some bookings from the UK dentists and their families. We’ve got some Aussie dentists coming along, and we don’t need massive numbers here.
We just need enough so we can put on a good show, but also we just need enough people to have some fun. This is actually a not-for-profit course. Me and Mahmoud are not doing this for profit. We just wanna have a jolly with our families and that’s straight from the heart.
I put the links in the show notes. You are gonna love this episode. Catch you in the outro.
Main Episode:
Dr. Masoud Hassanzadeh, welcome to the Protrusive Dental Podcast. You are speaking from the Netherlands right now. It’s so good to connect with you. Let me tell you and everyone how we ended up on here. I posted something about cracks on social media, and you said something so mind-blowing, so fascinating. I thought, I need to speak to this guy. Do you remember what you said? You mentioned—
[Masoud]
I know.
[Jaz]
You said we can heal cracks like bone. And so we’re gonna have to go there eventually because I’m really fascinated. Obviously there’s a bit of tongue in cheek there and whatnot, but I’d like to hear what’s the best thing we can do for cracks.
Many years ago, I did an episode with an endodontist, Krina, who’s wonderful. We talked about how much I hate cracks, because when you have a crack, there’s so many different ways it can go. The patient can become symptomatic.
We need to have a lengthy consent discussion with the patient that we don’t know how this tooth will react. We don’t know if it can be saved or not. There’s so much we can discuss, and I really wanna get into protocols and decision-making and the different philosophies of managing cracks.
So before we start with all that good stuff, Masoud, tell us about yourself. What are you doing in the Netherlands?
[Masoud]
Now I’m a dentist. I’m in the Netherlands, and it’s about four or five years that I have my own dental practice. I like restoring the tooth, and the crack was the first thing that actually I didn’t know what to do. When I asked other colleagues, they said, yeah, I also see them, but you can maybe put the primer, bonding on it, just flowable. Then someone said, yeah, you can put fiber on it. But it’s just confusing and there are a lot of controversies. Someone says, yeah, you have to pull it out.
Especially when the patient comes for small restoration, you say, okay, sorry, this is gone. I saw a crack. But it was really hard for me, and I just tried to do my best for the patients to save the tooth. This crack, it should have a philosophy. It should have a way of restoring it.
[Jaz]
Like protocols to go by based on the level of diagnosis. I think there’s only one thing that for sure we can agree with cracks, one thing, and then you tell me if things have changed. If someone has a true split tooth, i.e. the fracture’s going all the way through, obviously that’s for the bin, that’s for the forceps. So that’s one thing we’d agree with. And then also if you have like five, six millimeter probing depth associated with the crack, that’s hopeless prognosis, right? Unless we’re, let’s not beat around the bush, that is hopeless.
I think most of us get that and understand that. But then there’s that gray area where the crack is one or two millimeters subgingival, or the other gray areas. At what point do we intervene? Like we have MO amalgam and on the other marginal ridge we have a crack. This could be with staining, without staining, certain widths, certain durations, they’ve been there for 20 years. Knowing when to intervene for a crack is something I’d love to talk about with you today as well.
[Masoud]
So the first thing is we have to know the depth of the crack and where it is exactly. Is it in enamel, is it in dentine? And the second point is the age of the patient, because after age 40, 45, crack can unfortunately propagate very easily. All of the fracture cases which you see, most of them are elderly patients. Not young patients, unless there is a trauma, that’s another scenario.
These two things, especially the anatomy of the tooth and also thinking about crack repair, self-healing mechanisms, are really important for our decision-making for treatment. And also about the post that you shared, that was a huge crack. It starts from enamel, goes to the deep dentine.
[Jaz]
Can you remind me what my post was? I genuinely don’t remember. What was it?
[Masoud]
Really? It was an amazing image of a crack.
[Jaz]
Was it an extracted tooth in the crack?
[Masoud]
No, no, no. It wasn’t extracted tooth.
[Jaz]
Okay.
[Masoud]
It wasn’t extracted. It was just, I think intraorally you made the picture.
[Jaz]
Okay, okay. Like an MOD black crack running through like that.
[Masoud]
Yeah. And the initiation part was really open. You see just debris and a plug inside the crack.
[Jaz]
Let me see if I can pull this up because Protrusive Guidance audience, YouTube audience, it’s nice to have a visual. For those who are listening, of course we’re gonna describe it very clearly, and it’s a nice little starting point to discuss this one scenario. Yeah, that’s an awesome image. That’s the power of sandblasting, right? When you sandblast a crack, when you air abrade a crack, you can see it, and then I take a photo and I share with my patients.
So this post was all about how I communicate cracks to a patient. For those who are listening on Spotify, Apple, if you’re chopping onions, exercising, it’s just a really nasty crack when you remove an MOD amalgam and then you air abrade it, and you literally see the white air abrasion powder track all the way. So this is a very nasty crack, absolutely.
[Masoud]
You can see that this part is actually open, and your sandblast particle is just, how do you call it, it’s just—
[Jaz]
It’s jammed, it’s trapped in there.
[Masoud]
It’s like it’s trapped there. It’s just trapped.
[Jaz]
By open you mean we can feel it with the probe. Basically, with the probe we can actually feel.
[Masoud]
Yeah, so these are actually huge cracks and it is really hard to make a decision at this point. What are you going to do? Are you going to remove all this healthy tissue here to overlay that? Are you going to chase the crack? Are you going to follow it? Why should you follow a crack? I think these are very important questions to answer.
[Jaz]
Sometimes you’re looking, the patient’s got this non-specific pain. You’re like, could it be a crack kind of thing? A point you mentioned before we hit record: we only start noticing cracks when we wear magnification and we look really closely. Otherwise, we’re oblivious. We really don’t see these very obvious cracks because we’re not wearing magnification.
I also see everyone saying since COVID, we’re noticing so many more cracks. I think you are right, what you said earlier. Can you just say what you said earlier about how we are documenting better and stuff?
[Masoud]
There are studies that show just 8 to 9% of the cracks are symptomatic, like pain on biting or cold sensitivity. The other ones, like 80 to 90%, are just asymptomatic, so we just see them during restoration. Nowadays you see on Instagram, like the image that you shared, with high quality photography, with magnification, with microscope, with good images, most of the time the crack is the first thing that we notice.
It doesn’t feel good. Everyone says something is wrong with this tooth, you have to do something, and you can’t just put your adhesive system on it and put the composite or make a beautiful overlay on it. If you also check other posts, when there is a crack, there are always comments: how about the crack, what do you think, what’s the prognosis, what do you expect from your restorations? These are the things that you start to think.
When I started to learn about cracks, actually the studies were not from dentists. They were fracture mechanic engineering. They had the tooth and they just started to break it.
[Jaz]
Like flex it, load it.
[Masoud]
Flex it, see the strain and stress on the tooth and how it’s going to break. They gave us a lot of information about crack initiation and also crack propagation on a tooth. We also have some good studies from dentists. They try to treat it in different ways, especially the crack, and share their follow-up after five years and 10 years, which restorative restoration is just the best or restorative manner for many of the teeth.
[Jaz]
All these answers to be revealed in this podcast, I hope. So let’s start with the basics. One of my mentors, Lane Ochi, taught me that cracks in enamel are not so worry-ful. Cracks in dentine are the ones to worry about. So sometimes, let’s say you have a lower first molar. It’s got a DO amalgam, and on the mesial you see a crack. Now we see the crack obviously in enamel, and it could be stained or it could be not stained. But without removing the amalgam, how can you be sure whether it’s only in enamel or is going through the dentine?
[Masoud]
It’s hard. Maybe meta transillumination can give us information. Nowadays there is a new system. It is called quantitative percussion diagnostic, QPD, quantitative percussion diagnostic. They are giving very small percussions to the tooth, and they have AI information. If the percussion is 100, then it’s good, but if it’s 80 or 70, then there is a gap. There is an opening inside the tooth.
[Jaz]
It’s kind of like when you test, I don’t do this, but when you test an implant for integration.
[Masoud]
Yeah.
[Jaz]
It gives you some data. Oh, that’s so cool.
[Masoud]
Same system as it too. But it can be also because of a gap in a restoration. So if there is a gap, the information will change.
[Jaz]
False positive.
[Masoud]
Yeah. So the first thing is crack or the gap, but it’s still really hard. So always in old articles, the first recommendation is removing the existing restoration.
[Jaz]
I think that could be aggressive because there are some guidelines. For example, if you see a crack, and obviously like you said, 90% are asymptomatic, but if it’s not stained and you can just about see it with magnification but you can’t see it with the naked eye, then maybe that’s gonna be okay. But when it becomes stained, at that point we know that it’s big enough to allow stained particles and bacteria to go through. That is one thing I’ve seen cited in literature, that if it’s stained—
But my patients in their sixties, they all have cracks. If we chased every single crack, literally we’d be seeing like two patients a day and that’s all. That’s how I say it to my patients: you have cracks, exactly two cracks.
[Masoud]
It’s just, the crack belongs to tooth, so we have to know which crack, when we have to interact or not. Another point is use a fluorescence filter. Fluorescence filter shows us where bacteria are. So if you have a crack you doubt, you can just use the fluorescence filter.
[Jaz]
This is black light, this is like a UV torch, right?
[Masoud]
It’s not UV. It’s a fluorescence mode. You can have it on your microscope.
[Jaz]
Fancy microscopes.
[Masoud]
Yeah. There are also cheap ways, like in your loupes, or you can just have an extra oral light and then check it. If there is bacteria, the byproducts of bacteria become red, and in this way you can see if the crack is red or not, or is there bacterial biofilm in the crack or not. I also shared some posts about how you can check it, and that really makes it easy to check the cracks, and then you can start to remove it.
There is also a study from, I think, Ricucci, and he says when the crack is connected to oral environment, it is actually filled with bacteria and biofilm, especially if the crack is in dentine, because dentine is more flexible. It can open and close, so there is space for bacteria to invade. When it is in enamel, it’s more rigid, it’s harder. So the crack faces are mostly just touching each other. It’s called closed crack. In that way, there is almost no space for bacteria to invade inside the crack. That is also one of the reasons that we are not removing the cracks in enamel.
[Jaz]
But like you said, it’s difficult to tell. Let’s look at some metrics then, some clues. Some clues could be that the crack is stained, that we’re gonna use the fluorescent lighting to see if there is bacteria inside. But we also have to look at the patient. If they’ve got big strong muscles, if they’ve got a history of losing teeth before due to cracks, that is a very significant prognostic factor for me for should we treat this asymptomatic tooth or not. If they’ve lost teeth to cracks before, this is a really big deal.
Of course, if the opposing tooth has already been extracted, then that crack is not gonna propagate, so you don’t need to worry about that. You have to remember that this tooth, this crack is in the patient’s mouth, and look at the patient as a whole.
[Masoud]
Yeah, that’s right. I had a patient, she broke the second upper molar and there was no restoration on it, and it was just fractured. After three or four years, I saw a vertical crack on second upper molar. I said, yeah, we have to do something, otherwise you’re just going to miss this one. Indeed, big muscles.
[Jaz]
Big masseters.
[Masoud]
High force patient.
[Jaz]
These patients I’ve seen. I remember seeing quite a few. I document these cases really well because it always fascinates me when I get that. A few times a year I see a first premolar usually, or a second molar with a virgin crack without any restorations, and they come in irreversible pulpitis. It’s like, what’s going on? You start drilling into the tooth and you see this crack opening and opening and opening, and it’s fascinating.
They all have this thing in common whereby either their premolar is very cuspy, the angles are very acute in their premolar, and you can imagine that’s flexing. Steep cusps, that’s been a risk factor I’ve noticed. The other one is, of course, these clenchers, these high force patients with large muscles, because muscles matter. Force transmission will be different for each of these patients.
[Masoud]
Yeah, and also their distance to TMJ, because there is also a nutcracker effect. On the distal side of the second molars, upper and lower, we always see a vertical crack. Usually if the patient is like 50, 60 plus, just make an intraoral image and put it in the document of the patient. It’s always there. Also the upper premolar, because of its position, its anatomy, it’s just always going to break vertically from the furcation stress plane.
[Jaz]
Often see the palatal cusp completely come away, and then when you take that fragment out, you see four millimeters of root come out with it. I think all dentists have seen this. We get that a few times a year. It gives us another reason to remember that just because it’s asymptomatic doesn’t mean we should just leave it. We need to make a timely intervention.
So let’s circle on this and make some clear guidelines for dentists. Masoud, when should we be intervening? What’s the best evidence that we have so far about intervention? Obviously we spoke about patient factors, the muscles, the history, the anatomy of teeth, but any other guidelines: you can intervene when this happens?
[Masoud]
The first point will be symptomatic pain on biting. It’s called rebound pain because the fragment is going to move and dentinal fluid is going to fill the gap. During unloading, the fragment will come very fast and it will cause pain. If the crack is symptomatic, it should be treated because it shows that the crack is propagating.
The second one is also cold sensitivity. It can also be the same reason. The other ones are all dentinal cracks, especially if the patient is 40 plus, because dentinal cracks are structural cracks and enamel cracks are non-structural cracks. So if the patient is 90, there are a lot of cracks in enamel, we don’t need to treat them, only if the patient wants good aesthetics because the craze lines can get stained, become black, and maybe they don’t find it beautiful.
But the dentinal cracks are structural cracks and they can propagate. The reason is in its anatomy and histology, because dentine has its own mechanism to stop a crack. It’s not like dentine has no mechanism and the crack can just go. This crack can be there for 10 years, 20 years sometimes, but dentine has its own mechanism to stop the crack. At some point it’s not working anymore.
The reason is when the dentine tubule becomes closed, it is called sclerotic dentine, and all the collagens work together to create crack bridging to stop crack from propagating. But the collagens, when we get older, they are gluing to each other. It is called cross-linking. In that way, the crack can propagate more easily.
When there is a crack in a young patient, if he or she is not 40, I will not remove it. I will also check if there is bacteria or a plug inside it, but if not, I will just leave it there.
[Jaz]
Unless, and I love that you said that. However, I have this 19-year-old patient. She’s now 23, but when I first intervened on her, she was 19. She had that first rule that you said: she had symptoms. This is a high force patient, very rare to see a 19-year-old high force, huge masseters. Destroys her Essex retainers in a year. Now she’s wearing appliances, and it’s taken her three years to destroy that virgin crack in a molar, symptomatic. When I traced it, you can see the crack beautifully.
Once I restored it with a class II composite, because actually it didn’t warrant anything more than that, the similar thing happened a year later, symptomatic on the left symmetrical molar, and now things have been stable for some years. As a rule of thumb, yes, young patients’ dentine can probably handle it, but there are times where it may become symptomatic, and in that case we need to go case by case, I think.
[Masoud]
Yeah, and I think in that way we also have to remove the reason. What was the reason? Was it bruxism? Was it because of the anatomy of the antagonist or the tooth? Because there is a stress concentration in that point where the crack is started. So we have to distribute the stress in that place, in that plane. That is the important one. If we are just going to remove the crack and put the restoration on it, I’m afraid it’s just going to happen again.
[Jaz]
I love that you said this, and I’m nodding. What we had to do in this patient is, she had these crazy wear facets, so I had to do some adjustment. I had to do some selective grinding. This is force modulation. We might be removing microns of enamel to save millimeters of dentine and keep the teeth going as much as possible.
Instead of having the occlusion on a very steep incline, I had to flatten it a bit to make sure the stress distribution is better. I had this plunger cusp type on the opposing, I had to reshape it so it’s a bit more gentle. I had to remove a very steep incline and flatten it. I’m so glad you said that because if you just replace it, it will also have a marginal ridge fracture, which this one did, a tiny little marginal ridge fracture, which wasn’t a big deal, but it just goes to show that you have to do some sort of force modulation.
[Masoud]
Yeah, or maybe using nightguard.
[Jaz]
She does.
[Masoud]
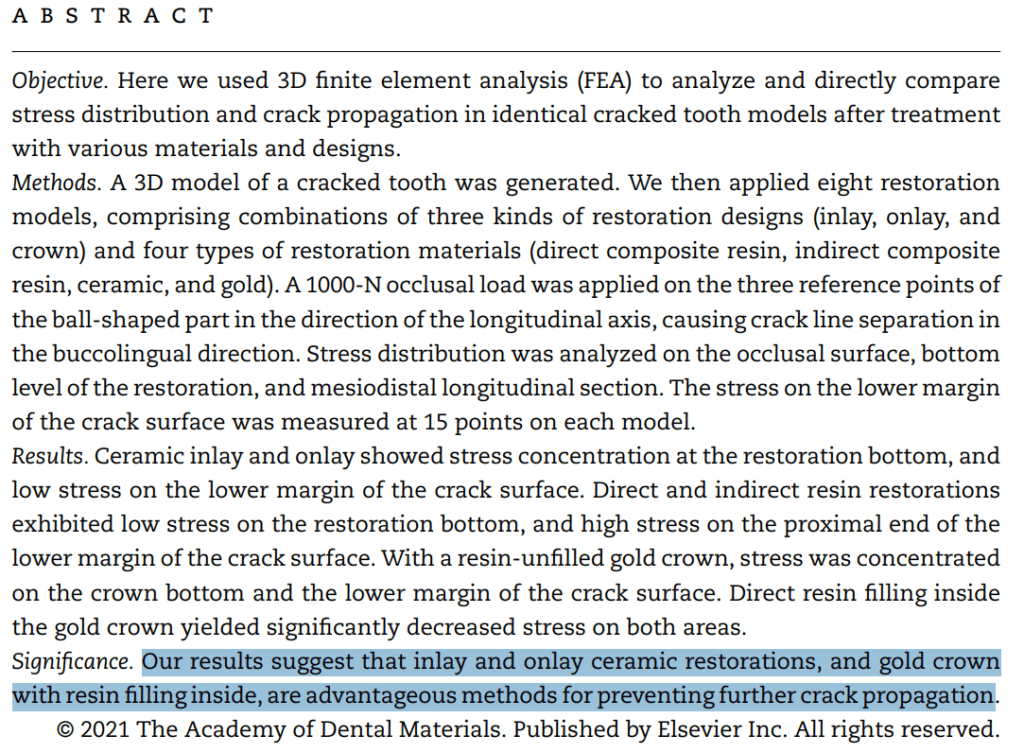
She’s a bruxist. I think also the final restoration is really important. There is a recent study from 2021. If the modulus of elasticity of the final restoration is close to enamel, the crack underneath will not propagate. It will just stop propagating. When you are restoring with composite, your modulus of elasticity is about 20–22 maximum, but the enamel is about 80. So if you use a restoration like a ceramic restoration, gold, with gold they also got good results.
I don’t know if it would be possible to share also these studies. I can send it to you.
[Jaz]
Oh, please. Our colleagues love to geek out on the studies. Send as many over. We’ll put it as a downloadable document.
[Masoud]
I will send it to you. They restored a cracked tooth with different kinds of restoration, and they checked when the crack is not going to propagate. They saw it’s happening when the modulus of elasticity of final restoration is close to the enamel. Actually the biomimetic concept: just try to mimic the nature.
[Jaz]
Like lithium disilicate, for example. In that specific patient, she was 19, so I did a direct. But if she was 20 years older, I would’ve gone for my usual protocol: good bonding under rubber dam with lithium disilicate, and maybe even at that stage be a bit more in terms of capping cusps where appropriate. We can talk about that as well.
[Masoud]
Yeah, because the form of the cavity is also important. In young patients, most of the time the cavity is not that huge. There is no place for indirect restorations. If it’s a small class I or really small class II cavity, I would also go for direct composite. But in huge restorations or multiple cracks, most of the time they’re just following each other and you see multiple cracks in one tooth. In that way, I think we have to choose the final restoration very clearly, a very good final restoration.
[Jaz]
So gold is approved, makes sense, and good bonding with ceramics. Are you including zirconia in that?
[Masoud]
Actually not, because zirconia has very high modulus of elasticity. It’s about 200 gigapascal and enamel is about 80. The second one is the bonding, because you lose your bonding strength in zirconia a bit faster than in lithium disilicate. These are the reasons that I’m not using zirconia. I’m using mostly lithium disilicate. But I see also dentists getting good results with zirconia and I understand that.
[Jaz]
Okay, fine. So we talked about which cases to intervene, why to intervene, why most of them are asymptomatic, but you gotta pick and choose the ones where it’s more likely to be in dentine. Look at the patient as a whole. Let’s talk about operative procedures: chasing cracks.
Back to the image that we shared, to what degree should we chase cracks? Because if you keep chasing, you’re gonna hit the pulp and then you’re gonna do an endo where you could have avoided the endo. That’s an easy one for us to understand. But are there any clear guidelines? We have caries removal endpoints. Do we have crack removal endpoints?
[Masoud]
That’s right. If it’s a non-vital tooth, I would remove all of it if it’s possible. If it’s a vital tooth, I will save the pulp. I will not expose the pulp. I will do my best to not expose the pulp. I will leave the crack on the center part and I will put fibers on it. In the peripheral zone, I try to remove it.
Unfortunately, most of these cracks are stopping at bone level, so it means that you have to deal with a very deep margin elevation or very deep margins. These are really hard to get a good adaptation between the matrix and the margin of the tooth. It’s really deep, it’s really dark, so you have to be sure that your light is going there for polymerization.
Most of the time they have a really high C-factor because it’s like a tunnel, a very narrow tunnel. The composite is going to shrink very badly. These are things that we have to think about: try to minimize the C-factor or the shrinkage stress and know that we have to deal with very deep margins.
The first reason that I am going to remove a crack is if it has a connection with oral environment, and if there is plaque there, it will invade inside. That will be the first reason. The second one will be crack propagation, because the crack tip has the most stress there. There are some studies, finite element analysis, if there is a crack, the crack tip is just red, all the stress is there, so it will propagate. By removing it, I can’t be sure that it’s not going to propagate anymore.
[Jaz]
I think to add to that, Masoud, I went through ebbs and flows of chasing cracks, not chasing, because I hear both camps. I hear what they’re trying to say. I think whenever there’s two extremes, you have to go down the middle and your answer’s somewhere down the middle.
Basic things like if you’ve got a crack on a marginal ridge, if you don’t at least address that crack, then that’s where you’re gonna get caries. It just makes sense. Also, you need to have access for your bur, access for your matrices. So that interproximal bit has gotta go, the proximal wall.
Then you’ve got to look at biological limits, pulp being one, but also connective tissue being the other. Kind of like how we don’t go into the pulp, the crack will get thin enough and you might accept, now the crack is thinner and I’m not gonna chase this anymore because you’ll compromise the restorative seal or result that you can get.
The other thing to consider there would be, when you are chasing these cracks, the most important part of the crack is the tip, like you said, that’s where the energy is. But if we can reduce the height of these cracks, we reduce the energy that goes to that tip. I think if you follow those principles of making the cavities cleansable, restorable, preserving pulp vitality, I think that’s a good middle ground.
[Masoud]
Yeah. So if I also adopt and I can’t remove it anymore, and it is white crack, I’m also stopping. Sometimes it’s so deep, my bur is not going to remove it anymore. I can’t touch it anymore. The good point is, thanks to the study of the engineers, when the crack is in root dentine, it’s not going to propagate that fast. Crack in coronal dentine propagates faster than in the root dentine, and this is really interesting.
[Jaz]
I didn’t know that.
[Masoud]
Yeah, I also didn’t know that. When it is in the root dentine, it’s just not going to propagate that fast. I will also share this study. I used all of this in my book. When I read it, I thought, this is mind-blowing.
[Jaz]
Well, let’s go to that thing then about healing cracks. You’re at that scenario where you’ve removed the height of it, you’ve cleared away the caries, you’re now not gonna expose the pulp, and you’ve reduced the height. You may be gonna cap some cusps, remove that couple millimeters of the cusp to make it lower in height so it’s less flexing. That all makes sense. But then at that point, how can we wave that magic wand and heal the crack like bone? You said we can heal the crack like bone. What do you mean when you said let’s heal the crack like bone can heal?
[Masoud]
When I read it for the first time, I thought, is it really possible? But it is possible. Like how there is a crack healing mechanism in the bone, there is also crack healing mechanism in the tooth. The difference is the crack healing mechanism in the bone is because of regeneration. You have a multi-step physiological process: inflammation and hematoma formation, bone remodeling, and at the end regeneration, and it is because of the blood supplies, because of the blood vessels there.
In the tooth, in dentine and enamel, we don’t have blood supplies. We don’t have blood vessels, only in the pulp. But interestingly, there is a crack healing mechanism in the tooth. It is different in dentine and also enamel. Knowing the histology and anatomy is really important.
The studies also show it is different in inner enamel than outer enamel because of the inorganic and organic matrix of the enamel: hydroxyapatite, the protein. The crack healing mechanism is different in inner enamel and outer enamel.
The first study is from 1949. He is called Sognnaes, 1949, and he thought the enamel tufts are actually cracks that are getting healed. Then no, it’s just hypocalcified intrinsic defect. After that, in 1994, Hayashi thought that there is mineral deposition inside the crack, especially enamel cracks, and these are medial cracks on occlusal part of the crack, and there is mineral deposition inside the cracks.
Myoung in 2009 saw even the protein-rich fluid can go to the crack and it can cause adhesive interlayer. It means two crack faces are going to glue to each other because of the protein-rich fluid. In 2013, Rivera and Arola, an engineering group, saw even that the length of crack is just going to decrease because of the healing mechanisms of the enamel of the crack.
[Jaz]
Increase the crack length?
[Masoud]
Decrease. Sorry, decrease.
[Jaz]
Okay, I’m with you. Now it’s making sense. It’s good to clarify. It shows you that I’m listening. Crack length is decreasing now, I get it. Now I’m totally on board.
Before we move on to dentine, you say all these wonderful things, but this is all just happening with saliva and the oral environment, or is there something we can do as dentists? Because we like to do things. How can we accelerate this? How can we create an environment conducive to enamel crack healing?
[Masoud]
That’s a good question. What’s the important point? It’s saliva. So be sure that your patient has not xerostomy. Stress can reduce saliva. That is the important part. After that, it is starting from the first moment that there is a crack. After 48 hours, they started to see that the crack is just decreasing, like it’s just healing.
Can I share that study with you?
[Jaz]
Yeah, talk about it.
[Masoud]
Indentation Damage and Crack Repair in Human Enamel.
[Jaz]
So it is legit. He’s not talking out of his ass. He’s being honest. This is cool. This is the geeky stuff we like on here.
[Masoud]
Look at this.
[Jaz]
We are seeing the crack length decrease after 48 hours. But this is in vivo or this is in vitro, like they extracted tooth?
[Masoud]
Yeah, this is extracted tooth. They don’t have it intraorally.
[Jaz]
You can’t measure that intraorally.
[Masoud]
No. I think intraorally, if they want to see, we have craze line and we have internal craze line. I think it would be possible to see that the internal craze line is going to get repaired, starting to get removed, disappear.
[Jaz]
There’s really nothing for us to do. There’s no special toothpaste. It’s just good to know that human enamel can have these self-repair mechanisms as long as you have a healthy patient, i.e. good saliva.
[Masoud]
Yeah, and also if we have a healthy pulp, because interstitial fluid has also effect on crack healing. Crack can propagate if it’s dehydrated, like in endodontically treated tooth, or when there is xerostomy. So it’s really important to keep the pulp vital.
[Jaz]
That’s what they say because it becomes brittle. All the chemicals that we use for root canal and everything, the tooth itself, when extracting a root filled tooth, it just feels different, feels more sclerotic, feels drier. That’s got to have something to do with it.
Fine. Then are we gonna talk about, is there any healing mechanism in dentine?
[Masoud]
There is also the healing mechanism in dentine, and it is also remineralization. The other very important point is the collagen matrix. The dentine is filled with the collagen matrix, and this collagen matrix is like a scaffold for ions, for phosphates and calcium, to come inside the crack.
The problem in dentine is because it’s flexible, so the crack is opening and closing, and that makes it really difficult for crack healing mechanisms. If the patient is old, 40 plus, the tubules become closed, so there will be no interstitial fluid to remineralize. Also the collagen matrix starts to glue to each other because of cross-linking, so there will be no scaffold for the ion transport. That will be the problem. Dentine has also its own mechanisms to get repaired.
[Jaz]
But there’s nothing we can do to promote this bone-like healing.
[Masoud]
No.
[Jaz]
And obviously most of the cases we see too late.
[Masoud]
Image you shared, there is no mechanism there. It’s really over.
[Jaz]
Well, let’s talk about that right here because you mentioned fibers. I don’t use fibers at the moment, but if there’s enough good clinical long-term evidence, I will. Of course I will join the party. You sound like you use fibers over cracks. Can you mention that? To someone who’s never used fibers and never done it justice by looking into it that much, I’ll be honest, what’s up with that? What are fibers doing? Is it robust enough? Is it strong enough? Do we have any good long-term data that the cases managed with fiber versus the case managed without fiber?
Obviously so many different variants and you can’t control for what the patient eats and clenching and that kind of stuff. But as a whole, where are we at with how far into its acceptance in the literature and acceptance into widespread practice we have these fibers, which we see so nicely on social media layering over these cracks in a criss-cross pattern?
[Masoud]
When there is a crack, there is a lot of stress there, so we have to do something. We have to redirect the stress. We have to distribute the stress, so it’s not just going to concentrate in one place. The fibers are the best way to do that. Putting the fibers on the crack.
In a vital tooth, the best way is laminating, like putting one piece of fiber on it. In an endodontically treated tooth, the best way is annular layering, like in a circle form shape inside the pulp chamber. There are two types: we can use glass fiber or we can use polyethylene fiber, the Ribbond. It’s about how they are, bidirectional or unidirectional. The fibers like Ribbond, we have to pre-wet it. It’s not ready to use. But the glass fibers are mostly treated, they are ready to use, and we can put it on the crack or where we want.
We can use fibers in dentistry in three ways. Strengthen the restoration: if it’s a huge composite restoration and financially it makes it a bit difficult for patient to pay for indirect, you can put fibers inside your restoration.
In that way you can strengthen your final restoration. We can protect the hybrid layer. The hybrid layer, the first minutes, is really sensitive to stress like shrinkage stress, and by putting fiber on it we can create a fail-safe protocol. It is not going to fail at that point anymore. And we can also strengthen the tooth, especially if there is a lot of sound tissue gone or removed, or if there is a crack, we can strengthen it with the fiber.
I recently read a study. They checked the fracture strength of natural teeth without restoration and also checked the fracture strength of a tooth with a crack, upper premolar. The intact tooth had about 1,200 Newton, but the tooth with the crack was about 400 Newton. So it was three times more brittle, it can fracture easier than the natural.
So in this way, with the fibers, you can redirect the stress which is coming to the crack.
[Jaz]
Do they have any such scenarios where they take that premolar and now chase out the crack as you would do, and then put the fiber on it, then restore it, and then put it under the same loading? It would be nice to know how many Newtons it can take. We’d expect it to be more?
[Masoud]
Yeah, it’s about 3,000.
[Jaz]
What?
[Masoud]
It’s about 3,000. You make it stronger than a natural tooth, actually.
[Jaz]
No way. You have to send this paper. That’s pretty cool. There’s process-based reasoning and there’s outcome-based reasoning. Process-based is like, by doing these fibers, by doing this, we’re strengthening the tooth. But what we care for more is outcome-based reasoning. For example, because we did this, my teeth are lasting 30 years, whereas before they were lasting 20 years.
We’re doing this more complex thing at an added expense, added time. We know there’s more risk involved in terms of you might mess it up, more time consuming and stuff as well. Whilst that sounds awesome, where on the benchtop we can get that data, and I think that says something, that’s pretty cool.
I didn’t know that, and I think there’s a lot of things in dentistry which we look at, we don’t have any clinical reasoning for, but it makes sense in a physics way, and a lot of occlusion is like that as well. A lot of the adjustments I do are based on that, so I’m not averse to it. But it’ll be nice to have any clinical data to support how it may be superior and therefore it can justify the added expense in terms of time and materials to a patient. Where are we now in terms of waiting for that kind of data?
[Masoud]
Not really that much. Endodontists are sharing more cases, more follow-ups, especially in crack removal. One is Philipson. I think I also had contact with him for writing my book. He shares that with removing the cracks, he sees that the teeth are going to live for 10 or 15 years, and this is why he’s supporting the idea of crack dissection. He’s dissecting the crack from 10 millimeters.
He says, okay, after dissecting the crack, there is the solid pocket from 10 millimeters. He’s putting Biodentine or MTA there. The x-rays look very crazy. I will never do it, but he just wants to save it. He made very good publications about it. It is really amazing to see how crack removal works.
But in terms of using the fibers and the long-term follow-ups, unfortunately I couldn’t find anything the way we have about the crown and cusp overlay, like removing all the cusps and onlay and then you see good results. We also have a study with crack removal, I think it’s an Australian study. It also shows in five years, 100% survival after removing the cracks.
[Jaz]
What do you mean by that? Sorry, 10% increase or 10% survival overall?
[Masoud]
They had no failure. The teeth were not extracted. All were just still in the mouth.
[Jaz]
They had 100% survival.
[Masoud]
100% survival.
[Jaz]
Okay, cool. But then that’s a very aggressive way. Based on what we’re learning from that study, should we be adopting that?
[Masoud]
That’s a good study. There are not that many studies. Unfortunately, like in adhesive dentistry you have thousands of studies. When you search about the primer or bonding, you get a lot of stuff.
[Jaz]
But in that case, you said they have to do endodontics, which makes sense. If you’re chasing all the cracks, you’re gonna be doing endo more often than not.
As Pascal Magne says, the root canal treated tooth will never win the Olympic Games of restorative treatment. Whilst that’s an interesting study, I don’t think I would change my way. I wouldn’t go too aggressive totally chasing all the cracks. Would you agree with that?
[Masoud]
Yeah, I would also not do it.
[Jaz]
In five years we need more, we need up to 20 years plus. We need to compare it to, is it better than what we’re already doing? I think you’ve mentioned some great points. Masoud, you’ve answered all my questions. It was really fun to speak with you. I would love for you to tell us about your book. You mentioned your book a few times. I’ve seen it on social media. Tell us about it, because it is no easy feat to do a book. I’m doing a book at the moment. I know it’s no easy feat. Tell us about it.
[Masoud]
Yeah, this is my book, The Cracked Tooth.
[Jaz]
Oh, sweet. Is this a different one to the one that you had on?
[Masoud]
No, this is the one. I also published another one that was the Glossary of Biomimetic Restorative Dentistry.
[Jaz]
That’s the one I saw. Oh yeah, that’s the one I saw. Okay, cool.
[Masoud]
This is a new one from this year. This is only about cracks in tooth and what we have to know about it, with all references at the end of each chapter.
[Jaz]
That’s amazing. Oh man, that’s so geeky. I love that, Masoud. Well done. That must have taken so much time and effort. Really well done, mate.
[Masoud]
Yeah, it took almost three years to do it. First I had to study a lot and I had to make all the connections with the engineers. Actually, how does it work? I really didn’t understand. There is a Paris law in fracture. In that way they can measure crack propagation, but the problem is they have a continuing mechanism. It means point A and point B have the same chemistry and physiological properties, but in the tooth each half millimeter is different.
So it makes it really difficult for the engineers to calculate the real crack propagation in a tooth. They have to divide it to deep dentine, intermediate dentine, superficial dentine, inner enamel and outer enamel. With my book, my idea was making a very small book at 90 pages to share with my colleagues, to share my information with them, but it became 400 pages. Still there are studies, some of them I read some weeks ago and I said, maybe I should put this study also in my book.
[Jaz]
Volume two, that kind of stuff. Masoud, is this on Amazon?
[Masoud]
This is on Amazon, yeah.
[Jaz]
Alright. Please send me the link. I would love to share it with Protruserati. I think what you said was making a lot of sense. I like that. The only unanswered question I have is the very first few things you mentioned about the percussion-based diagnostics. Is that like a special tool you have to buy?
[Masoud]
Yeah. It is called InnerView. The links are very interesting. The first dentist who called the crack in dentine structural was David Clark. David Clark wrote a study in 2003 with Challis, and Challis invented this instrument. It is called InnerView. In this way, you can measure if there is a crack in a tooth or not. I will show image of it.
[Jaz]
I like the idea of gaining objective data. It’s why I bought the T-Scan in occlusion. I like the timing data, the force data. This is another thing that can help you, like transillumination, to get more data of should you intervene, should you not. I like that.
[Masoud]
Yeah, it is really—
[Jaz]
Is it an expensive toy, Masoud?
[Masoud]
Yeah, I think it’s about two or three thousand.
[Jaz]
Yes, it’s an expensive toy.
[Masoud]
Two or three thousand dollars.
[Jaz]
Is there an AliExpress version? No, I’m just kidding.
[Masoud]
I know there is a first version and another team tried to make it, but it’s not that easy to use. The idea of InnerView is you have a pen and you’re going on each tooth and you can test it.
[Jaz]
It’s like you’re describing a Tooth Slooth in a way.
[Masoud]
Yeah, like that. But this one is going to tap or send a percussion on the tooth and get the info back from the tooth. It is now waiting for ADA approval from USA. I think they’re waiting this year or next year to bring it to the dental shops.
[Jaz]
Amazing. Now that I know about this pricey device as well, this data is cool. I didn’t know about that before. I didn’t know that root dentine is more resistant to cracking. That was fascinating. I didn’t know about the epic impact of these fibers on these extracted teeth. That’s really cool to know. I didn’t know you had that book on cracked teeth. That is awesome, and I’ll put the link there for everyone to check it out, to see all your hard work.
Masoud, thanks for sharing so generously with the community. We really appreciate people like you doing the work that we don’t want to do, all the hard work and reading, then sharing all the answers with us. We really appreciate you. You’re the kind of guy whose homework we copied.
[Masoud]
Thank you.
[Jaz]
Thank you so much, Masoud, for all your work on cracked teeth, and I’ll put all the papers that you send in the blog link. I’ll put your Instagram. Please tell us about your Instagram.
[Masoud]
On Instagram, I started just sharing normal things. I had just 100 followers. Then I started to share my daily challenges. Look guys, this is the thing that I am dealing with and I have to do. Now it’s about 400, 500 posts that I made with really difficult situations, and I always get good answers or good reflections, feedbacks: hey, you are sharing the things that I maybe didn’t know how to do. Now I have more ideas.
With the last years, I make all the images with the microscopes. They are 28, 29 times magnified. It gives more information. You can really see the mantle dentine. You can really see the inner enamel. You can see the outer enamel.
You can see the histology difference between these two, also where we call the dentinal enamel junction. I also share images with fluorescence mode, fluorescence filter. You can see where the bacteria are and where you have to remove. Not all the length of the crack is filled with bacteria. When it is closed crack, there is no room, even in dentine.
I shared a case when I started to chase the crack, and each millimeter I made the image with fluorescence mode. You see after two or three millimeters, it’s not red anymore, it’s just clear. But the crack is still there. So it means the crack spaces are so tight connected to each other, so there is no space.
[Jaz]
So it’s like the width of the crack is getting less, which makes sense. The crack would be higher, more open at the top, and as you go more cervical, it would get thinner and thinner, and that makes sense.
[Masoud]
It is called transition. We have three types of cracks. One is closed crack. All the crack faces are just connecting, like crack in enamel. Second one is transitional crack. These are like the first point, the initiation part is open, but close to the tip the crack is closed. The other one is totally open crack. In dentine, we see most of the time transitional crack. The first point is open, and near the crack tip it’s closed. When it’s open, there is space for bacteria and biofilm to go there.
[Jaz]
Amazing. Everyone, do check out Masoud’s Instagram. I’ll put the link below. Masoud, thanks so much, my friend. Have a delightful Friday, and I can’t wait to publish this. I’ll give you a shout out, my friend. Thank you so much.
[Masoud]
Thank you. Thank you. Thank you, Jaz, for your time, for invitation, and sorry for messing up a bit with the increasing and decreasing.
Jaz’s Outro:
It’s totally fine. I was thinking in my head, okay, when’s the right time to intervene? And you nailed it. Thanks so much for a wonderful summary on cracks.
Well, there we have it, guys. Thank you so much for listening all the way to the end. I know you want the papers. Scroll down below. If you’re on Protrusive Guidance, they are all there.
If you’re on YouTube, check out the WordPress link and again, we will have them all there for you to download. The easiest way is to head to protrusive.co.uk/cracks. That’s protrusive.co.uk/cracks. Our manager, Alex, is going to zip all these papers that Masoud sent us and send them to you. We’ll also send you a link to his book on Amazon. I think it’s amazing that he’s done this, and if you wanna geek out with him more, check out his book. I’ll also put his social media.
Of course you can get CE for this. You’ve done the hard work. You’ve listened, you’ve watched, you can get CPD or CE credits. We are a PACE-approved education provider. The only way to get CE for this is on the Protrusive Guidance app. You need at least the CE plan, which is amazing value. Dentists are getting 100 hours of CE every year just from listening to the podcast while they’re commuting and answering the quiz on the app.
If you wanna get the full fat version and get access to Vertipreps for Plonkers, the 21-day Photography Challenge, Rubber Dam, premium clinical walkthrough videos, all that good stuff is on the Ultimate Education Plan. Check it out on the Protrusive Guidance app.
Once again, if you’re fancy coming to Dubai with us, it’s globaldentalevents.co.uk. You click the button to get a quote. You have to say how many people are coming. Is it you and a spouse, or you and spouse and kids, or just you?
Then you get some hotel options and flight options, that kind of stuff, and you get a quote that’s going to be tax deductible because it’s for work. Remember we are going to learn occlusion and have some fun. So globaldentalevents.co.uk. I’ll put the link, everything you need in the show notes.
Thank you so much for listening all the way to the end. Honestly, it means so much to have your listenership and engagement on all the platforms, including Instagram and stuff. Thank you so much and catch you, same time, same place next week. Bye for now.
