Cardionerds: A Cardiology Podcast
Cardionerds: A Cardiology Podcast 339. ACHD: Electrophysiology in ACHD with Dr. Frank Fish
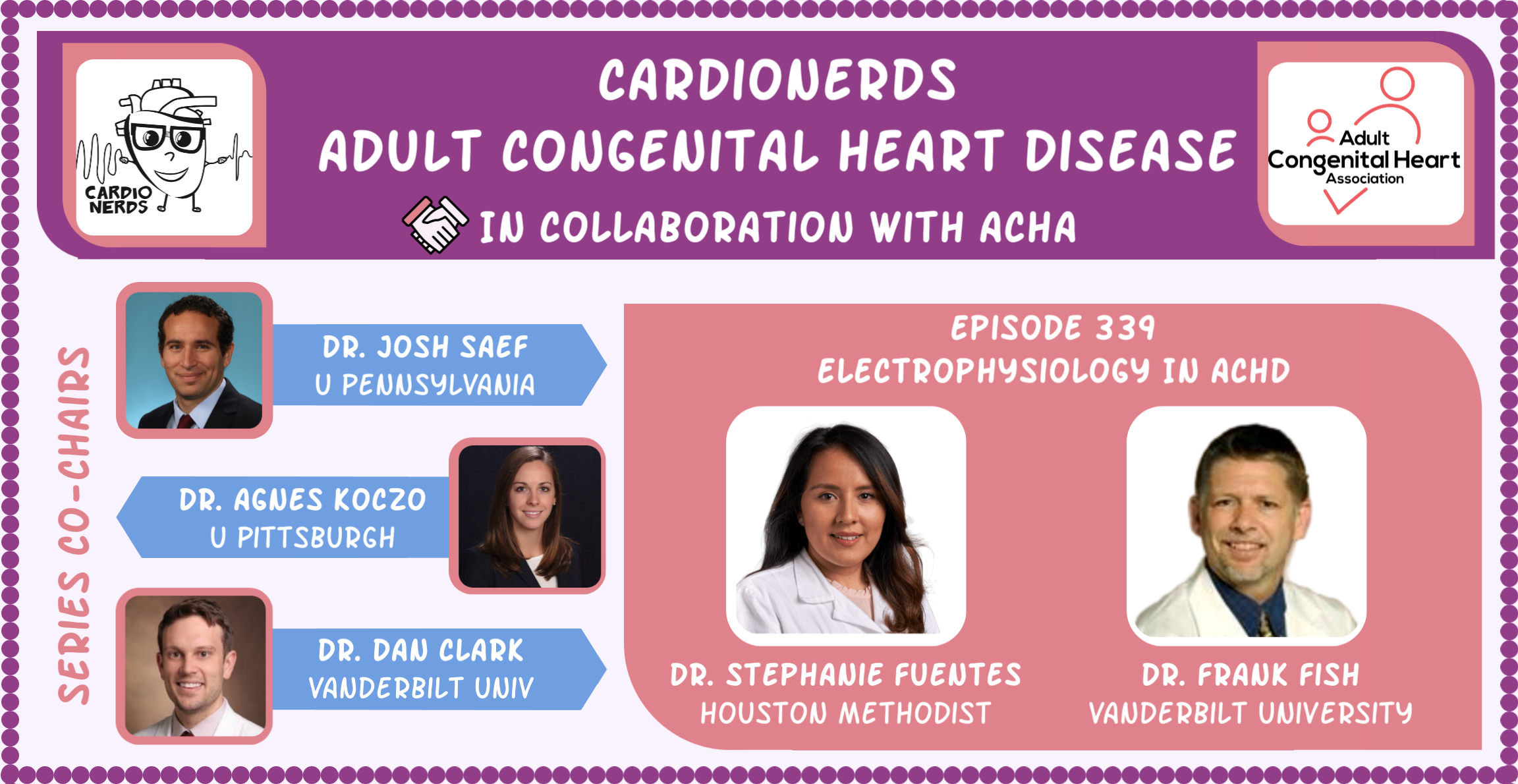
CardioNerds (Amit Goyal and Daniel Ambider) ACHD series co-chair Dr. Daniel Clark (Vanderbilt University), cardiology FIT lead Dr. Stephanie Fuentes (Houston Methodist Hospital), and Dr. Frank Fish, a Pediatric Electrophysiologist and the Director of the Pediatric Electrophysiology (EP) Lab at Monroe Carrell Jr Children’s Hospital at Vanderbilt University. He is a board certified Adult Congenital Heart Disease (ACHD) physician and has a wealth of experience performing EP procedures in adults living with congenital heart disease. Audio editing was performed by student Dr. Shivani Reddy.
In this episode, we discuss key concepts and management of electrophysiologic issues that we can encounter when caring for adults with congenital heart disease. Arrythmias in adults with congenital heart disease can be intrinsic due to the defect itself or as a consequence of the interventions that they have undergone to palliate and/or repair these defects. The complex anatomy of these patients and the years of pressure and volume load make them not only exquisitely hemodynamically sensitive to arrhythmias (that may otherwise not be of much consequence to the general population) but they also make interventions (catheter ablation or device implant) complex. We therefore embark in a case-based discussion of patients with ACHD (Fontan circulation, Ebstein’s anomaly and Tetralogy of Fallot) in an effort to highlight the presentation of arrythmias and the management strategy in this very important group of patients.
US Cardiology Review is now the official journal of CardioNerds! Submit your manuscript here.
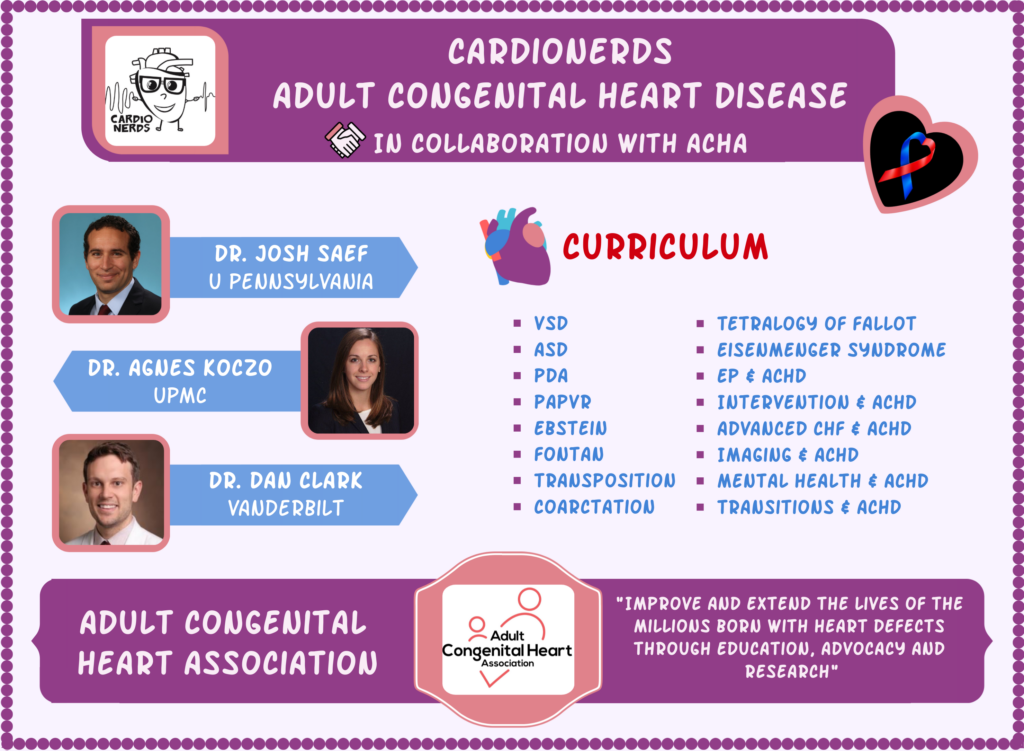
The CardioNerds Adult Congenital Heart Disease (ACHD) series provides a comprehensive curriculum to dive deep into the labyrinthine world of congenital heart disease with the aim of empowering every CardioNerd to help improve the lives of people living with congenital heart disease. This series is multi-institutional collaborative project made possible by contributions of stellar fellow leads and expert faculty from several programs, led by series co-chairs, Dr. Josh Saef, Dr. Agnes Koczo, and Dr. Dan Clark.
The CardioNerds Adult Congenital Heart Disease Series is developed in collaboration with the Adult Congenital Heart Association, The CHiP Network, and Heart University. See more
Pearls – Electrophysiology in ACHD
- Patients with Fontan circulation have a high risk of developing atrial (and ventricular) arrhythmias and they are highly sensitive to the hemodynamic consequences that these arrythmias ensue. The goal of therapy then should be to achieve sinus or atrial paced rhythm. Rate control should NOT the goal.
- Patients with Ebstein’s anomaly have high arrhythmic potential. They can have multiple accessory pathways (especially right sided) which can in turn be associated with sudden cardiac death. We should have low threshold for EPS +/- catheter ablation in patients with WPW pattern.
- Patients with Tetralogy of Fallot have a unique risk for SCD that warrant ICD implant apart from the standard criteria (LVEF <=35% and NYHA II-III symptoms). This involves the pump (RV dilation/dysfunction), electricity (QRSd>180 ms) and surgical repair approach.
- Patient’s anatomy is the major consideration when implanting devices (PPM/ICD). We ought to assess for residual intracardiac shunt at the atrial level and consider closing if feasible prior to placing a device. CRT has merit in systemic LV but less so in systemic RV.
Notes- Electrophysiology in ACHD
What should we know about atrial arrhythmias in a Fontan patient?
- Intraatrial re-entrant tachycardia (IART) is slower than typical atrial flutter with atrial rates generally <300 bpm. It does not have typical flutter waves and when it is slow enough, it may be confused with sinus tachycardia. A simple maneuver to help discern between sinus tachycardia or AT/AFl is to stand the patient up. If there’s no variability in heart rate, then it is less likely for it be sinus. With intact AV conduction, atrial flutter or IART can conduct 1:1.
- IART is usually a harbinger of issues among patients with Fontan circulation. These patients are dependent on passive pulmonary blood flow. So, loss of AV synchrony in these patients may raise left atrial pressures, impede forward flow and subsequently compromise cardiac output. Tachycardia reduces diastolic filling, thus further limiting systemic venous return. IART can be associated with systemic illness, worsening pump function, obstruction in the Fontan circuit, etc. Once it’s present, it warrants full investigation into the trigger and a management plan to prevent recurrence.
How should we manage atrial arrhythmias in a Fontan patient?
- The goal of therapy is to achieve sinus (or A-paced) rhythm. Rate control should not be the goal.
- If hemodynamically unstable-> DCCV
- Chemical options include ibutilide but would use with caution if one does not know sinus function as post conversion bradycardia can put patient at risk for torsades. Amiodarone or Procainamide are helpful in patients that are requiring frequent cardioversions acutely. However, would avoid amiodarone if patients are heading to EP lab for catheter ablation as this medication affects defibrillation thresholds.
How should we approach catheter ablation in a Fontan patient?
- Catheter ablation should be considered in centers with expertise with managing ACHD patients.
- Operators should understand patient’s anatomy, ventricular function and systemic issues such as renal or hepatic function. Prior to intervening, venous/arterial access issues ought to be assessed. In cases where there’s femoral vein or IVC occlusion, trans-hepatic approach can be considered. Presence of atrial thrombi ought to be assessed prior to ablation as well. Given slower atrial rate leading to less degree of stasis compared to Afib, left atrial thrombi are less common.
- When ablating, first assess the Fontan itself (lateral tunnel in this case) as it can become dilated overtime and this leads to an area of scar that can be source of arrythmias. If Fontan is not the source, then one has to go through it to reach the atria. In extra-cardiac Fontan, this may require the use of a radiofrequency-powered needle to cross the conduit and thereby reach the atria. A retrograde approach from the aorta, into the systemic RV, and then into the atria is much less ideal given that this would entail placing catheters in the systemic circulation for prolonged periods of time, raising thromboembolic risk, not to mention the trajectory that is required with this approach.
How should we approach anticoagulation in Fontan patients?
- CHADS2VASC for CVA prevention risk stratification is not as heavily applicable in this patient population as compared to the general population.
- The Fontan circuit is highly susceptible to thrombosis. Each element of Virchow’s triad is present in patients with Fontan circulation: (1) Venous stasis – from the passive pulmonary flow and venous hypertension necessary to maintain this forward flow, (2) Activation of blood coagulation – underlying liver disease, prostheses, and inflammation may all play a role in making these patients hypercoagulable, and (3) Venous damage – surgical reconstruction of the venous tree and chronic venous hypertension lead to venous damage. Together, all these factors increase the risk of thrombosis. Let’s not forget that there are often residual right-to-left shunts that present opportunities for paradoxical emboli to the systemic circulation. So, not only is clotting more common, the stakes are often higher in this population.
- All adults with Fontan palliation are on at least anti-platelets (aspirin) and many on systemic anticoagulation. Special circumstances that prompt consideration of systemic anticoagulation include prior clots in the Fontan circuit, atrial arrhythmias, thrombi in hypoplastic chambers when there are systemic communications or if they have other indications like: DVT/PE, mechanical valve prosthesis.
What arrhythmias are associated with patients who are born with Ebstein’s anomaly and when should we pursue EP study and/or catheter ablation?
- Approximately 1/3 of adults with Ebstein’s anomaly have multiple accessory pathways (particularly right sided) and atrial tachyarrhythmias are very common in these patients.
- In the setting of ventricular preexcitation (Wolf Parkinson White syndrome), atrial tachyarrhythmias may expose the patient to a higher risk of lethal ventricular arrhythmias. This is why we don’t give nodal blockers to WPW patients in atrial fibrillation, as this can precipitate 1:1 conduction down the accessory pathway. In patients with Ebstein’s anomaly, without WPW, EKG shows right bundle branch block.
- Ventricular myocardium that lies between the true AV groove and displaced tricuspid valve is thin-walled and unhealthy thus prone to ventricular tachycardia
- The 2018 ACC/AHA ACHD guidelines give EPS with or without catheter ablation a IIA indication for diagnostic evaluation of adults with Ebstein anomaly and ventricular preexcitation (WPW pattern), even without SVT. Likewise, these guidelines give a IIA indication for EPS +/- CA prior to surgical intervention on the tricuspid valve regardless of a history of preexcitation or SVT.
In which ACHD patients should we consider the use of Holter monitor when they are asymptomatic?
- To screen for abrupt loss of pre-excitation in patients with Ebstein’s anomaly.
- In Fontan patients to screen for junctional rhythm as this loss of AV synchrony would lead to long term hemodynamic consequences.
- In patients with tetralogy of Fallot, to identify patients with non-sustained VT
- In patients with D-TGA and atrial switch, to screen for sinus node dysfunction
- In patients with CC-TGA, to screen for AV conduction abnormalities.
How should we approach ICD implant for primary sudden cardiac death prevention in patients who are born with Tetralogy of Fallot (ToF)?
- In general, primary prevention ICD for ToF is indicated for patients meeting standard criteria (LVEF <=35% and NYHA II-III symptoms). There have been many studies to better understand SCD risk among patients living with ToF. We can think of the risks in 3 categories: (1) The pump – how hypertrophied, dilated, and/or weak is the RV? Is RV dilatation so bad it is affecting the LV? If so, this confers a greater risk of SCD. (2) Electrical – has the patient had prior VT/VF (are we talking secondary prevention?)? How wide and fractionated is the QRS? We think of QRSd >=180 msec as a cut-point for increased risk and there’s new data from France last year that a fractionated QRS may matter even more (DAI-T4F registry). (3) Surgical/RVOT – what was the original repair? Did they use an LV vent or a RV ventriculotomy? Was there a transannular patch or RVOT aneurysm post-operatively? What’s the current status of the pulmonary valve?
What are the technical considerations that ACHD patients warrant when having an ICD/PPM implanted compared to the general population?
- Patient’s anatomy is the major consideration when implanting devices. We need to first assess if there’s remaining intracardiac shunting at the atrial level and consider closure prior to implanting a device.
- CRT has merit in systemic LV. CRT in systemic RV like patients with D-TGA with atrial switch has less merit and is more technically challenging as it may require epicardial lead.
References – Electrophysiology in ACHD
- Stout KK et al. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation.2019;139:e698-e800. Doi:10.1161/CIR. 0000000000000603
- Khairy P et al. PACES/HRS Expert consensus Statement on the recognition and management of arrhythmias in adult congenital heart disease. Heart Rhythm.2014(11): e102-e165.
- Baumgartner H et al. 2020 ESC Guidelines for the management of adult congenital heart disease, European Heart Journal. 2021; 42:563-645 doi:10.1093/eurheartj/ehaa554
- Walsh EP, Cecchin F. Arrhythmias in adult patients with congenital heart disease. Circulation. 2007 Jan 30;115(4):534-45.
- Waldmann et al. Long-Term Follow-Up of Patients With Tetralogy of Fallot and Implantable Cardioverter Defibrillator: The DAI-T4F Nationwide Registry. Circulation. 2020 Oct 27;142(17):1612-1622. doi:10.1161/CIRCULATIONAHA.120.046745.Epub 2020 Oct 1.
Meet Our Collaborators!
Adult Congenital Heart Association
Founded in 1998, the Adult Congenital Heart Association is an organization begun by and dedicated to supporting individuals and families living with congenital heart disease and advancing the care and treatment available to our community. Our mission is to empower the congenital heart disease community by advancing access to resources and specialized care that improve patient-centered outcomes. Visit their website (https://www.achaheart.org/) for information on their patient advocacy efforts, educational material, and membership for patients and providers
CHiP Network
The CHiP network is a non-profit organization aiming to connect congenital heart professionals around the world. Visit their website (thechipnetwork.org) and become a member to access free high-quality educational material, upcoming news and events, and the fantastic monthly Journal Watch, keeping you up to date with congenital scientific releases. Visit their website (https://thechipnetwork.org/) for more information.
Heart University
Heart University aims to be “the go-to online resource” for e-learning in CHD and paediatric-acquired heart disease. It is a carefully curated open access library of educational material for all providers of care to children and adults with CHD or children with acquired heart disease, whether a trainee or a practicing provider. The site provides free content to a global audience in two broad domains: 1. A comprehensive curriculum of training modules and associated testing for trainees. 2. A curated library of conference and grand rounds recordings for continuing medical education. Learn more at www.heartuniversity.org/